A challenging case: A dog with a painful red eye
This dog's problem was not conjunctivitis-as was first thought-but something much more serious.
A 7-year-old 19.8-lb (9-kg) intact female Scottish terrier was presented to the Colorado State University (CSU) James L. Voss Veterinary Teaching Hospital for evaluation of redness and pain of the right eye of four days' duration.
HISTORY
Just before the onset of the problem, the dog had been playing outside, but there was no history of known trauma. The dog had been taken to an emergency clinic soon after the red eye had been observed. The emergency clinic veterinarian had diagnosed conjunctivitis and had also found a grass awn in the left ear, which was removed. He had prescribed a triple antibiotic ophthalmic ointment to be given in the right eye two or three times daily.
Over the next three days, the eye seemed to worsen, and the dog became lethargic and depressed. Thus, the dog had been taken to its primary veterinarian who had immediately referred it to CSU. The CSU emergency service saw the dog and immediately triaged it to the ophthalmology service.
EXAMINATION
The results of a full physical examination showed no abnormalities except in the right eye. The eye had profuse mucopurulent ocular discharge, and the eyelids and conjunctiva were markedly swollen (Figure 1). The dog was in extreme pain and screamed when the right eye was touched, which made ocular examination and retropulsion difficult.

Figure 1. An eye with endophthalmitis similar in appearance to this case. Note the marked amount of thick mucopurulent discharge with a grossly abnormal cornea that is hazy and yellow to a degree that an examination of the anterior structures of the eye could not be performed.
The right cornea appeared to be yellow-tinged, and a small amount of free blood had collected in the ventral fornix. In addition, a 4-mm, round fibrin clot on the outside of the cornea was present in the ventral fornix near the area of hemorrhage. These changes precluded our ability to evaluate the anterior chamber, pupil, or posterior ocular structures. The intraocular pressures were 33 mm Hg in the right eye and 7 mm Hg in the left (normal = 15 to 25 mm Hg). Despite the lower than normal intraocular pressure, the left eye had no signs of uveitis (e.g. flare, miosis) and was considered normal. The lower intraocular pressure was considered to be age-related. The dog was deemed blind in the right eye because there were no indirect pupillary light reflexes from the eye nor were there tracking or menace responses. There was no obvious foreign material in the conjunctival sac of the right eye, although a thorough examination was difficult.
PRESUMPTIVE DIAGNOSIS
Because of the severe pain the dog was experiencing, our assessment of probable permanent blindness, the increased intraocular pressure that indicated glaucomatous damage, and the history of possible foreign body exposure, we made a presumptive diagnosis of septic endophthalmitis. We recommended removing the eye immediately. The owner agreed to the transconjunctival enucleation.
SURGERY
Blood was drawn for a complete blood count and serum chemistry profile for a preoperative evaluation; the results of these tests were normal. Preoperative medications included fentanyl (4 µg/kg intravenously), atropine (0.04 mg/kg subcutaneously), and diazepam (0.5 mg/kg intravenously), and anesthetic was induced with intravenous propofol (2 mg/kg). The dog was intubated and placed on isoflurane gas maintenance.
The eye was minimally clipped and then aseptically prepared with dilute (1:30) povidone-iodine solution and draped. A retrobulbar nerve block was performed to help control postoperative pain. The block consisted of injecting a total of 2 ml of a 1:1 mixture of bupivacaine (0.5%) and epinephrine (1:200,000) behind the eye through a 22-ga needle.
A lateral canthotomy was performed for better exposure to the globe, and the nictitating membrane was removed. The eye was dissected out of the orbit by using curved Metzenbaum scissors and a combination of blunt and sharp dissection. Upon ventral dissection, a large amount of purulent, foul-smelling material began to seep from the surgical site, but no ocular perforation was identified despite careful inspection. The purulent material was removed with sterile 4-in-x-4-in gauze sponges. The four rectus muscles, retractor bulbi muscles, and the optic nerve were sharply cut, and the eye was removed.
Postorbital fat and soft tissue were removed from the orbit, and it was inspected carefully for signs of a mass or foreign body. None was seen. Because of the contamination from the purulent material, the orbit was flushed numerous times with sterile saline solution (total of 300 ml). Because of client financial contraints, bacterial culture and sensitivity testing was not performed.
A meshlike web of 3-0 nylon suture material was anchored to the periosteum of the dorsal and ventral orbital margins to prevent the skin from sinking into the orbit. The eyelid margins were trimmed with Mayo scissors. The remaining palpebral margins were brought together by using 3-0 braided absorbable suture material in a simple continuous pattern, and the skin was closed with 3-0 nylon suture material in an interrupted cruciate pattern. The enucleated globe was submitted for histologic examination.
Recovery from anesthesia was uneventful, and the dog was sent home the same day. The owner was given instructions regarding antibiotic and pain control medications: 20 mg/kg amoxicillin trihydrate-clavulate potassium, 4 mg/kg tramadol, and 2 mg/kg carprofen given orally twice a day. An Elizabethan collar was placed on the dog to prevent self-mutilation of the surgery site.
FOLLOW-UP EXAMINATIONS
The dog returned to the referring veterinarian two weeks after the surgery for suture removal and recheck. The dog had recovered well, and all medications were discontinued. A follow-up at CSU two months after the surgery showed that the dog was happy and healthy.

Figure 2. Subgross image of the eye in cross section, stained with hematoxylin-eosin. The eye is no longer intact, with the posterior sclera containing a full-thickness defect (asterisk). Inflammatory cells have diffusely infiltrated and accumulated (seen as dark purple) in the vitreous cavity and in the surrounding orbital tissue.
HISTOLOGIC FINDINGS
Histologic examination findings of the globe were consistent with a diagnosis of septic panophthalmitis secondary to an intraocular plant foreign body. Hemorrhage, fibrin, and large sheets of neutrophils were present in both the anterior and posterior chambers and the vitreous cavity. The retina, choroid, and sclera were effaced by neutrophils and variable amounts of edema and hemorrhage, and a full-thickness defect was present in the posterior sclera (Figure 2). In the vitreous, a piece of plant material was surrounded by coccoid bacteria that, in turn, were surrounded by neutrophils (Figure 3).
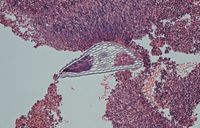
Figure 3. In one area of the vitreous cavity, a small bit of plant material is seen with a dense surrounding of bacteria and inflammatory cells immediately adjacent to it. The plant material is multichambered with a refractile cellulose wall.
Neutrophils and smaller numbers of lymphocytes and plasma cells infiltrated the extraocular muscles and periorbital fat. The myofibers of the affected extraocular muscles were shrunken and hypereosinophilic and had pyknotic nuclei. Moderate numbers of neutrophils infiltrated the cornea, which was diffusely ulcerated. The posterior scleral defect was thought to be the site of penetration of the foreign body as no other fibrous tunic defects were identified.
The final diagnosis was septic panophthalmitis due to plant foreign body penetration of the globe.
DISCUSSION
Intraorbital and intraocular foreign bodies are not uncommon in dogs1-6; however, this case of an intraocular foreign body is unusual because the plant material probably entered the eye through the posterior sclera rather than anteriorly through the cornea. Most ocular foreign bodies in dogs enter the conjunctival sac and are removed by increased tearing and blinking, go down the nasolacrimal puncta, or enter the orbit by migrating between the globe and the orbital wall.1 Once in the orbit, the foreign material typically causes orbital cellulitis or abscess formation.1,2 Grass awns (foxtails) and other plant materials are the most common intraorbital foreign bodies seen in dogs, although glass and metal (air gun pellets) objects3 and porcupine quills4 have also been reported.
Intraocular foreign bodies usually penetrate the eye directly; however, migration of objects from the orbit through the sclera have been reported.3 One report described the case of a Kerry blue terrier that was presented for anorexia, fever, facial and throat pain, and chemosis and episcleral congestion of the right eye.3 Oral antibiotics failed to resolve the problem. After heroic efforts to save the eye failed, enucleation was performed. Histologic examination of the globe showed severe, destructive panophthalmitis. Plant foreign material was detected in the globe. The presence of a posterior area of disruption in the sclera suggested that it was the most likely route by which a grass awn had entered the eye.3
Another article reported on a series of five cases of dogs that had ocular or orbital porcupine quills.4 Two of the dogs had only orbital lesions, one had a corneal perforation that ruptured the lens capsule, one had a corneal lesion but the quill did not reach the lens, and one had an intraocular and intraorbital quill. In the dogs with intraorbital lesions, it was suspected that the quills entered the orbit or eye through the roof of the oral cavity.4
Diagnosis
Intraocular foreign bodies are diagnosed based on a combination of appropriate history, clinical signs, and ocular imaging. As in the case presented here, there may be a history of the dog running through grass, and grass awns may have been found in the ears or coat or between the toes.
Clinical signs usually start as conjunctival and episcleral hyperemia, prolapse of the third eyelid secondary to enophthalmos (due to pain or a retrobulbar mass), blepharospasm, and epiphora. The signs frequently progress to severe hyperemia, mucopurulent discharge, possible exophthalmos, and severe pain around the face and upon opening the mouth. The dog is often febrile, anorectic, and depressed.
In this case, the clinical signs and history were compatible with a diagnosis of infectious panophthalmitis, and the dog was blind and in severe pain. Thus, a grave prognosis for saving the eye was given, and enucleation was performed without further diagnostic tests. Other causes of panophthalmitis in dogs include deep fungal infections or ophthalmomyiasis interna.7 A diagnosis of ophthalmomymiasis carries a fair prognosis because the larvae can be surgically removed if caught early.7 However, if panophthalmitis develops, salvaging the eye is unlikely.
In cases in which intraocular foreign bodies are suspected, the signs are less severe, and the eye potentially retains vision, ocular imaging techniques should be used to better determine the feasibility of salvaging vision. That is true in cases of suspected intraorbital foreign bodies, as well.
Ultrasonographic examination of the globe and orbit is the most useful technique for determining the amount and type of damage.8 Glass, metallic or plastic objects, and porcupine quills can be easily located with ultrasonography since these objects prevent penetration of the ultrasound waves beyond them and, thus, cast a hypoechoic shadow.8 On the other hand, organic material cannot be imaged as well since it is often of a similar consistency as the tissue around it. However, ultrasonography is valuable in these cases as it can detect prognostic indicators such as retinal detachment and the status of the lens capsule. When information is needed about the complete orbit and globe, a combination of modalities is recommended since intraocular structures are better seen with high-resolution ultrasonography, while periocular structures are better imaged with magnetic resonance imaging (MRI).9
Computed tomography (CT) and MRI are frequently used to detect intraocular foreign bodies in people. In a study comparing these two techniques, MRI was able to accurately detect eight of eight nonmetallic foreign bodies (wood, glass, plastic, rock) planted into enucleated sheep eyes while CT was able to detect seven of eight.10 CT was unable to detect the wood foreign body. Both techniques could resolve objects as small as 3 mm. If a metallic foreign object is suspected, MRI is contraindicated since the magnetic field will attract the metal and potentially traumatically extract it from the tissue.
Prognosis and treatment
The prognosis and treatment of a canine eye with intraocular foreign bodies depend greatly on the initial damage done to the eye, the type of material present, the duration of time from insult to treatment, and the skill of the person treating the eye.
If the foreign body has only penetrated the cornea and has not reached the lens and the trauma is recent, its removal, corneal repair, and topical and systemic antibiotic therapy are indicated. In addition, treatment for the resultant secondary uveitis should be initiated with topical atropine and nonsteroidal anti-inflammatory drugs. Without direct involvement of intraocular structures and given prompt, appropriate therapy, the prognosis is good.
If there is perforation of the sclera and uvea, retinal damage is likely to be present. In these cases, referral to a veterinary ophthalmologist is highly recommended. The prognosis in cases of perforation depends greatly on the location of the object within the eye. If the object can be readily removed from the eye surgically (e.g. if it is in the anterior chamber), the prognosis for vision is good. If it is in the posterior segment, the prognosis—even with surgery—is guarded to poor. However, resolution of hemorrhage and surgical retinal reattachment is possible.4
If perforation of the lens capsule has occurred, a guarded prognosis must also be given. Rapid leakage of lens proteins induces phacoclastic uveitis, which is often progressive and can destroy the eye. Immediate diagnosis and aggressive anti-inflammatory treatment along with the surgical removal of the lens is necessary to have any chance at all of saving the eye.4 Thus, emergency referral to a veterinary ophthalmologist is important in most cases of ocular perforation. If an eye containing a foreign body is blind and painful, enucleation should be performed as soon as possible.
In some cases, it is possible to leave the foreign material in the eye and retain vision.5 In a series of case reports of four eyes of three dogs containing lead shot, intensive antibiotic and anti-inflammatory therapy was used to control the signs and prevent infection. All dogs recovered but not without sequelae, such as cataracts, retinopathies, and posterior synechiae. The fact that the foreign bodies in these dogs was made of lead afforded a better prognosis since "inert metallic foreign bodies with smooth edges such as gunshot are well-tolerated in the anterior chamber, iris, vitreous, and lens."5
In people, the most common intraocular foreign bodies are metal from hammering metal on metal.11 These foreign bodies usually enter the eye through the cornea and progress to varying depths within the eye. Because most of these metallic objects are small, reported immediately by the patient, and, thus, removed rapidly, there is a good prognosis for a positive visual outcome. In a retrospective study of 59 people undergoing foreign body removal, the best results were obtained when there was vision at the time of presentation, hammering metal on metal was the mechanism of injury, and surgical removal, which included vitreous removal (vitrectomy), was within 24 hours.12 Poor prognostic factors were absence of vision at presentation, posterior location of the foreign body, and large size of the foreign object.12 Unfortunately, because dogs are unable to report trauma to their owners and are prone to larger intraocular foreign bodies than people are and because of the relative paucity of veterinarians who are able to do posterior ocular segment surgeries, the prognosis is much worse in veterinary patients.
Juliet R. Gionfriddo, DVM, MS, DACVO
Department of Clinical Sciences
College of Veterinary Medicine and Biomedical Sciences
Colorado State University
Fort Collins, CO 80523
Thomas Chen, DVM
Department of Clinical Sciences
College of Veterinary Medicine and Biomedical Sciences
Colorado State University
Fort Collins, CO 80523
REFERENCES
1. Brightman AH, McLaughlin SA, Brogdon JD, et al. Intraorbital foreign body in the dog: a case report. Vet Med 1985;80:45-48.
2. Brennan KE, Ihrke PJ. Grass awn migration in dogs and cats: a retrospective study of 182 cases. J Am Vet Med Assoc 1983;182:1201-1204.
3. Bussanich MN, Rootman J. Intraocular foreign body in a dog. Can Vet J 1981;22:207-210.
4. Grahn BH, Szentimrey D, Pharr JW, et al. Ocular and orbital porcupine quills in the dog: a review and case series. Can Vet J 1995;36:488-493.
5. Schmidt GM, Dice PF, Koch SA. Intraocular lead foreign bodies in four canine eyes. J Small Animal Pract 1975;16:33-39.
6. Sandmeyer LS, Bowen G, Grahn BH. Diagnostic ophthalmology. Anterior uveitis, cataract, retinal detachment, and an intraocular foreign body. Can Vet J 2007;48:975-976.
7. Ollivier FJ, Barrie KP, Mames RN, et al. Pars plana vitrectomy for the treatment of ophthalmomyiasis interna posterior in a dog. Vet Ophthalmol 2006;259-264.
8. Morgan RV. Ultrasonography of retrobulbar diseases of the dog and cat. J Am Anim Hosp Assoc 1989,25:393-399.
9. Penninck D, Daniel GB, Brawer R, et al. Cross-sectional imaging techniques in veterinary ophthalmology. Clin Tech Small Anim Pract 2001;16:22-39.
10. LoBue TD, Deutsch TA, Lobick J, et al. Detection and localization of nonmetallic intraocular foreign bodies by magnetic resonance imaging. Arch Ophthalmol 1988;106:260-261.
11. Greven CM, Engelbrecht NE, Slusher MM, et al. Intraocular foreign bodies: management, prognostic factors, and visual outcomes. Ophthalmology 2000;107:608-612.
12. Chaudhry IA, Shamsi FA, Al-Harthi E, et al. Incidence and visual outcomes of endophthalmitis associated with intraocular foreign bodies. Graefes Arch Clin Exp Ophthalmol 2008;246:181-186.