Clinical Pearls for the equine eye exam
Vision and comfort are best assessed in the undisturbed patient in its familiar environment.
General examination of the eye is a routine part of equine practice, both to determine the cause of ocular pain and as part of a prepurchase examination.
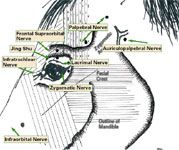
Figure 1: Lateral schematic of the head. Peripheral nerve blocks are highlighted. Lidocaine is deposited with a 25-gauge needle. Deeper nerves require a 1.5-in. 22-gauge needle.
This article features some new technology together with useful techniques that greatly enhance the ease and amount of information obtained, as well as safeguarding the damaged globe. While the general principles to be described are familiar to all equine specialists, there are some clinical pearls that can greatly enhance your satisfaction and ultimate confidence in clinical findings, yielding more rapid resolution.
The eye has been the source of wonder to many for generations, yet it induces frustration and anxiety for veterinarians. Our intention within the scope of this article is to encourage and stimulate interest in the eye. Remember, there are many practical and simple additions to your approach that are rewarding. Be warned, however; this is addictive!
Restraint
Most normal horses and those with minor injuries often will permit an ophthalmic examination in their stall with minimal restraint. When transported to the hospital or examined under more difficult circumstances, additional restraint is necessary to protect the eye, the examiner and to permit a thorough evaluation. Painful globes are a profound sensory stimulus, and a variety of techniques might be required to examine a potentially ruptured globe.

Figure 2:(a) Cross section through the eyelid showing correct placement of the lavage system to avoid corneal contact. (b) If the lavage is closer to the eyelid margin, it may abrade the cornea during blinking, and result in ulceration. (c) Note incorrectly positioned lavage system, which may result in a corneal ulcer.
When serious injury is suspected, sedation should be performed before handling. Xylaxine (Rompun®) at 0.3-0.6 mg/kg IV is usually sufficient if the patient has not been overly stimulated. It is imperative that adequate effect is permitted before proceeding, otherwise, further sedation is difficult to achieve.
Routinely, I wait five minutes to 10 minutes after the initial head drop to avoid a rapid rebound when the eyelids are touched. Peripheral nerve blocks also are useful. More profound sedation can be achieved with detomidine (0.015-0.025 mg/kg, IV). Supplementation with butorphanol may be useful in particularly painful patients, but is frequently complicated by head tremors and jerky motions. Standing the horse in a stock is very helpful if profound sedation is to be used. Acepromazine is minimally effective. I prefer to avoid manual restraint with a twitch unless the examination is a brief recheck, or a mild supplement to sedation is required. Dosages might require adjustment for miniature horses, warmbloods and draught horses.
Peripheral nerve blocks
The most commonly performed nerve block is the palpebral nerve (branch of the auriculopalpebral, a division of the facial VII), which provides motor innervation to the powerful orbicularis oculi muscles in both eyelids (Figure 1). Complete blockade results in a flaccid upper eyelid, which can be raised without resistance. The palpebral nerve traverses the zygomatic arch at its peak 8-10 cm from the dorsal orbital rim, and again at 2-3 cm, and it may be palpated or strummed through the skin. A 25-gauge needle is inserted so that it is subcutaneous beside the nerve, and 1-2 mL lidocaine 2 percent is deposited. Substantial resistance to injection indicates that the needle is intradermal. The lidocaine may be fanned out with the needle, or the area can be rubbed subsequently to disperse the drug. Both of these techniques irritate horses. Nerve branches arborize while approaching the eyelid, so more peripherally fewer branches will be blocked, and greater residual muscle tone is encountered.
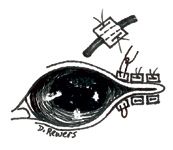
Figure 3: Temporary tarsorrhaphy placed laterally, either with or without a stent. Examination of the cornea is reduced, but enhanced corneal protection is provided.
Other branches arise around the orbital rim from the facial nerve, and to achieve complete paralysis, a more proximal auriculopalpebral nerve block is performed posterior to the dorsal ramus of the mandible using a 22-gauge 1.5-in. needle buried to the hub and depositing 3-8 mL lidocaine. Longer-acting anesthetic agents are less desirable because of the longer interval until normal blinking. Topical ointment is a logical supplement at the conclusion of the examination to prevent dessication of the epithelium.
Skin sensation around the orbit is provided via two divisions of the trigeminal nerve (V): through the lacrimal n., infratrochlear n. and frontal n. (ophthalmic division) and the zygomatic n. (maxillary division). The frontal and supraorbital nerves are the same. The sites for blockade are shown in Figure 1, p. 6E. A head jerk is often experienced if the needle impinges on sensory nerves. If inserted swiftly without the syringe, skin resistance will prevent its inadvertent removal during head motion. When the head is still, the syringe is attached and the lidocaine injected. Small vessels accompany the nerves, and blood may be seen in the hub. Gray horses appear to bleed more, and their hair color makes it more evident. Occasionally, a small hematoma may form, but rapidly reduces with light pressure. Desensitization is useful for surgical repair, and familiarity with the topographical areas assists in diagnosing traumatic damage to sensory innervation.
The infraorbital nerve exits the infraorbital foramen just anterior and dorsal to the facial crest between the globe and the nostril, underneath the levator nasolabialis muscle. This nerve is blocked occasionally to remove trigeminal (V) sensation in the evaluation of head-shakers, but has a more-practical use in that its desensitization permits suturing wounds of the nostril and lip. A 20-22 gauge needle is inserted directed caudally into the foramen, or its vicinity and 3-10 mL lidocaine are deposited. The block may require 20-40 minutes to achieve full desensitization.

suggested reading
A more advanced technique is the retrobulbar block, which is most commonly performed under general anesthesia. It prevents strabismus, extraocular muscle tension during ophthalmic surgery, and if coupled with 1-2% v/v epinephrine (1:1000) it limits hemorrhage if enucleation will be performed. Specific descriptions are available in current texts. It may also be performed under standing sedation, with caution and dexterity. The eye should be protected from inadvertent trauma. Temporary blindness should be anticipated if the optic nerve is blocked.
Examination and diagnostic skills
An ocular exam is most likely to identify more subtle abnormalities when performed systematically on each occasion. Vision and comfort are best assessed in the undisturbed patient in its familiar environment or under the conditions (bright light or darkness) where the complaint arises. Indicators of discomfort include reduced palpebral fissure size or asymmetry (compare eyelash and vibrissae angle), ocular discharge, increased blink rate, prominence of the nictitans, and the horse's avoidance of contact with either globe. Palpebral fissure asymmetry is noteworthy and can reflect abnormalities with the orbit, globes or eyelids. Vision testing should include the menace response from multiple angles, and a navigation (maze) test before sedation. Visually oriented responses, such as avoiding objects and stepping over kerbs indicate vision, is present: partial visual impairment is more challenging to identify.
Eyelid innervation and motor function is verified by the palpebral response (prior to blockade), and direct and consensual pupillary light reflexes (PLR) are assessed with a bright light. Both rate of constriction and degree of completeness are assessed because partial denervation is relevant. Apparent lack of menace can be caused by eyelid paralysis, but nictitans excursion often confirms an intact visual pathway. Anisocoria is assessed in dim lighting by observing the tapetal reflection outlining the pupils through the direct ophthalmoscope from 5-8 feet in front of the head. Buphthalmos or phthisis bulbi should be differentiated from globe displacement (enophthalmos or exophthalmos) and relative nictitans prominence. Asymmetry might be due to ocular pain (globe retraction), reduced orbital contents (enophthalmos), physical displacement by a mass, phthisis bulbi/globe rupture, autonomic denervation (Horner's syndrome) or eyelid paralysis, and less commonly fracture or other damage to the orbit.
The corneal reflection should be bright and sharply focused, indicating tear film quality and quantity. Dry eye is rare in horses but might be associated with skull trauma, plant intoxication and infrequently with pharmaceutical intoxication or eosinophilic keratitis. Corneal clarity and discoloration are important findings and are more easily identified in dim surroundings. A generalized haze might reflect focal or geographic corneal edema, ulcerative keratitis, fibrosis or aberrant metabolic products such as lipid or mineral. Opaque focal white-tan opacities within the cornea are particularly significant (see stromal abscess in previous edition).
Fluorescein stain retention is best identified with cobalt-blue light. More subtle tear film and epithelial abnormalities are seen with Rose bengal stain and bright white light [Akorn Inc., (800) 535-7155]. Lissamine Green stain is less useful. Corneal staining should be performed before iatrogenically drying the tear film and causing false positives. Magnification and focused light beams allow closer scrutiny. Fundic abnormalities can occur in 10 percent of horses, so indirect screening funduscopy should be performed routinely, ideally after dilation, but few lesions are solely in the periphery. The fundus includes the ONH, retina and highly vascular choroid, which dorsally contain the reflective tapetum fibrosum. Direct ophthalmoscopy permits close examination of the optic nerve head (ONH), but the 7.9x magnification and reduced field of view make a complete exam laborious. Indirect ophthalmoscopy can be performed more rapidly with a bright light source and indirect lens (20D magnification 0.79x, or 14D magnification 1.2x). Apparent lesions should be interpreted with other ipsilateral changes and contrasted with the fellow (or other normal) eye.
Many normal variations are encountered, especially among subalbinotic horses. The entire length of retinal vessels (1-2 ONH diameters) might not be seen unless the room is dark. The remainder of the retina is perfused perpendicularly by choroidal capillaries, the "stars of Winslow". If the RPE is unpigmented, dramatic views of the choroidal vasculature are apparent and should be differentiated from hemorrhage. Typically well-organized parallel vessels are completely normal unless the overlying retina has been depigmented by some pathologic process.
Many aging changes pose little threat to vision but should be considered together with the clinical complaint and demonstrated ability to navigate and perform visually oriented tasks.
The PanOptic® (Welch Allyn) is a new device which provides intermediate field-of-view and magnification while still being operated with one hand. It is monocular and lacks stereopsis, but it permits more rapid screening of the fundus. The more powerful lithium battery is recommended for adequate illumination because of the internal lenses. An extended rubber eyepiece reduces ambient illumination, but many horses resist its contact with the eyelids. This device provides a single instrument alternative to screening with indirect ophthalmoscopy, and scrutiny of potential abnormalities by direct funduscopy.
Enhanced views of the cornea and anterior chamber are obtained with a slit lamp, which permits focused circular and rectangular light beams to illuminate transparent structures, demonstrating more subtle abnormalities in the cornea. An inexpensive version with several useful features is available from Heine USA. The best optics and optical detail require a more-sophisticated, dedicated instrument such as the Kowa SL-15, but its cost is more prohibitive. Many direct ophthalmoscope heads have a slit aperture, which may be used as a reasonable substitute to determine the depth of corneal lesions when observed indirectly. In dim surroundings, the light is positioned directly in front of the globe with the slit box brought into focus on the corneal surface, and the defect depth is assessed by observation from an oblique angle (not using the ocular). The same aperture can be used to enhance depth perception on retinal examination, observing through the instrument eyepiece.
Laboratory tests
Corneal culture should be performed whenever focal corneal discoloration is present. The culture can be discarded later if unnecessary, but its early acquisition ensures an unadulterated sample. Lid blockade, or topical desensitization may be used if necessary to acquire the sample. If the culturette touches the eyelashes or skin, it should be discarded and another sample acquired. Fungal culture requires specific requests at most laboratories: It should be ordered if cytology is suggestive of hyphae. Sensitivity testing should be ordered concurrently with the culture.
Cytology may be acquired after corneal desensitization using a blunt instrument at the edge of the lesion. The sample should be applied cautiously to several slides, permitting in-house review, as well as submission if indicated. Routine staining is adequate with oil-immersion to identify the commonly encountered pathogens. Surgical blades and scissors should be used only on the cornea with great caution. Melting ulcers can present with a prominent focal excursion from the cornea: resecting this area may result in corneal perforation and require immediate surgical repair. In preference, cytology acquired at the lesion edge is usually much safer and equally useful. Corneal cytology will be reviewed in greater detail in a future article.
Serology samples may be acquired in uveitis patients for Leptospira sp. and other testing. This is perhaps more relevant in recurrent episodes. The results can be useful ancillary aids but are seldom diagnostic in their own right.
Subpalpebral lavage system
In severe ocular disease, and nervous individuals, chronic therapy will be considerably easier, more effective and tolerable for the patient and handler with a subpalpebral lavage system (SPL). The SPL can be placed conveniently during the same sedation as the exam, if it is performed expeditiously. If the patient is too alert, additional sedation is desirable.
Preparation for the SPL placement includes palpebral and supraorbital (frontal) nerve blockade, local anesthesia at the intended site of skin perforation, topical desensitization and local cleansing. The corneal and conjunctival surfaces are rinsed with dilute povidone iodine (0.2% iodine), which may be applied from a spray bottle. This is irritating to the conjunctiva in horses, and may be flushed with sterile saline.
Several SPL models are available, but I prefer a pre-assembled system (Lavage kit #6612 or #6612L, Mila International, 888-MILA INT). These kits contain almost all the items necessary to place and retain the system. The University of Florida recommends the longer, three-foot lavage line, and a more-secure administration port is assembled by inserting a 22-gauge 1.5-in. intravenous catheter into the distal tubing, adding an injection cap and taping the device securely to a wooden tongue depressor secured to the mane. The lavage is sutured to the skin of the skull with 2.0 nylon using the supplied plastic stops, or through zinc-oxide tape shaped into a butterfly. Sutures are placed to avoid peripheral nerves and to establish a curvilinear track to the forelock, then to the mane.
The lavage line is placed close to the neck skin, and braided in place, finally being covered with the mane. In polo ponies, the lavage line may be shortened and taped to the halter. The line should lie straight but not be overly tight. The subpalpebral lavage disc, which retains the position, is extremely unlikely to become separated unless substantial pressure is applied.
Lavage placement
There are several useful pearls while placing the lavage. Profound sedation is very helpful, permitting first-time placement. The patient's reaction increases substantially with each additional attempt. The needle is slid under the eyelid guarded by a gloved finger until the orbital rim is palpated. If the patient reacts, a Q-tip or finger may be placed initially, and SPL placement may be resumed when the patient again acclimates. Elevating the eyelid reduces the working space and frequently results in incorrect placement. Ensure that no wrinkles of conjunctiva are entrapped on the stylet point to avoid placement in the middle (moving portion) of the eyelid (Figure 2). The lavage line will not move if it is seated within 2-4 mm of the orbital periosteum and sits safely in the dorsal fornix. Corneal ulceration is a complication if the soft tip is permitted to abrade the epithelium during blinking (Figure 2). When positioned for skin puncture, the needle should be held firmly at the distal end to swiftly traverse the eyelid in one pass. I prefer the skin puncture to be at the mid-point of the dorsal orbital rim, where it closely coincides with the acupuncture point Jing Ming. This site can provide chronic low-grade analgesia, and certain individuals appear more comfortable almost immediately, beyond that anticipated with sedation alone. Ensure that no knots are present in the coil of lavage line before threading the needle. Alternatively, the lavage may be placed through the inferior eyelid, or even retrograde within the nasolacrimal duct, although both of these methods require that medication must move against the flow of gravity. Attention to aseptic technique minimizes the risk of eyelid abscessation. Oral antibiotics may resolve a small reaction at the site rapidly, but profound blepharitis indicates the SPL should be repositioned. Minor fibrosis almost always occurs, and granulation is common at the site of the SPL egress through the skin but rapidly resolves after removal. Careful maintenance allows extended treatment periods of four weeks to eight weeks. Sparing amounts of vaseline or other viscous barrier ointment will limit persistent open sores resulting from epiphora and excess medication causing facial wetness and irritation beneath the lower eyelid.
When correctly placed, the flaccid eyelid should not move when the lavage line is pulled. If it does, the cautious action is to reposition the SPL while the stylet is still sterile. A printed area on the tube should be visible adjacent to the eyelid, and allows the client to monitor the lavage position.
Medications are administered analogous to the use of an intravenous catheter. The injection cap is replaced periodically. Syringes with swaged-on small gauge needles (such as insulin syringes) minimize dead space and medication wastage, and extend the life of the injection cap. Dose volume of 0.15-0.2mL is adequate for most patients. I prefer to slowly propel each medication with air and ensure its delivery. An alternative is to sequentially load each medication in the line, allowing the latest medication to propel the oldest. Potential disadvantages are inexact dosing and risk of medication loss. Self-contained pumps may be added to the system to provide continuous irrigation of the ocular surface with ophthalmic solutions. Ophthalmic suspensions and viscous products, such as natamycin (antifungal) and serum should be followed with a solution to prevent obstruction of the line. The major disadvantage of pumps is that individuals most in need of such continuous care typically need more than one medication. A three-way stopcock may be added to allow additional intermittent therapies as desired. The additional expense of the system is rapidly recuperated with more accurately delivered medication, reduced frustrations, and more rapid recovery. Few clients later regret the placement of an SPL, but many wish the it was present from the beginning of medication.
Mechanical protection
Protective facewear is helpful to prevent rubbing of the cornea. Hard-cup hoods are ideal but produce tremendous sweating in hot climates. Additional ventilation holes may be bored to reduce sweating. Fly masks are often sufficient to prevent rubbing, but a determined horse can still do damage while wearing a fly mask. Cross-tying is highly effective for individuals who are accustomed to it, but is not recommended otherwise. Rapid control of uveitis with NSAIDs and atropine substantially reduce the impetus to rub. Stall confinement is recommended, and horses with an SPL should be permitted limited turnout under constant observation. Similarly, commingling with other horses is likely to result in SPL damage.
Temporary tarsorrhaphy is a very useful adjunct therapy to protect against rubbing, and to provide a support to the cornea after surgery (Figure 3). It is also useful where facial paralysis prevents normal eyelid motion, such as after lateral facial trauma or head entrapment in a confined space. Tarsorrhaphies may be placed in the standing sedated horse with local nerve blockade, a line block and sufficient caution to avoid iatrogenic injury to the globe. It is critical to ensure that the suture emerges from the center of the eyelid margin and not any nearer to the conjunctiva, otherwise corneal ulceration will result. Sutures may be tied as simple interrupted or horizontal mattress, using 5.0 silk or smaller material. A stent may be crafted out of IV tubing, a rubber band or foam if desired. I prefer 1 or 2 simple interrupted sutures without stents, tied in the lateral one-third of the palpebral fissure.
Medication format
Most ocular pathologies are treated easily with topical ointment, providing extended contact time and ease of administration. More-serious injuries might require frequent administration, and the build up of the petroleum base reduces the drug's contact with the cornea and hence its effectiveness. Epithelialization of indolent-type corneal ulcers may also be reduced by ointment coating. Ointment induces a severe endophthalmitis if it enters the anterior chamber, for example if a deep corneal ulcer perforates. Ointments should not be administered to cases of iris prolapse.
When ophthalmic solutions are preferable, the most certain application is via a SPL. Infrequent administration can be achieved by loading 0.15-0.2 mL of solution into a 1-mL or 3-mL syringe with a 25- or 27-gauge hub (no needle), and gently spraying the corneal surface while protecting the hub end. Few individuals will permit direct administration from the dropper vial, but rotating the head facilitates this technique in tolerant individuals. Multiple drops should be administered.
Subconjunctival administration of solutions provides a local depot, which can supplement topical medication. Drugs can cross the sclera to the anterior chamber, or leak from the injection site back onto the cornea. A very small-gauge needle should be used to minimize leakage. Particular caution is necessary with corticosteroids. In the event of an infected ulcer, the depot might require surgical excision. Additional formats, such as encapsulated slow-release devices might become more popular in the future. A cyclosporine device can be implanted beneath the sclera to provide excellent control of uveitis in many ERU patients.
Dr. Cutler is a staff ophthalmologist with the Animal Eye Specialty Clinics in West Palm Beach and Wellington, Fla. He is a consultant to the equine specialists at Palm Beach Equine Clinic in Wellington and Reid and Associates in Loxahatchee, Fla. He is board certified by the American College of Veterinary Internal Medicine and by the American College of Veterinary Ophthalmologists. He received his veterinary degree from the Veterinary College of Ireland, University College Dublin, and his MS degree and residencies at the University of Florida. His interests include equine corneal disease and surgery, particularly transplantation. Visit his clinics' web sites at www.animaleyedocs.com and www.equineclinic.com