Essential information for veterinarians about hemangiosarcoma
A renowned veterinary oncologist outlines the current knowledge about this cancer of the blood vessel walls, from presentation to prognosis.
Hemangiosarcoma is often the first thing that comes to mind when a splenic mass is found in a dog. Although hemangiosarcoma is the most common malignant splenic tumor, it is not the only differential. Unfortunately, obtaining a definitive diagnosis and prognosis requires histopathology that must be obtained surgically. The decision to proceed with surgery in the face of a potentially poor prognosis can be a difficult one for clients, especially in an emergency, where the tumor has ruptured and is actively hemorrhaging.
During a session at the 2020 American Veterinary Medical Association Virtual Convention, Sue Ettinger, DVM, DACVIM (oncology), an oncologist at VCA Veterinary Referral and Emergency Center in Norwalk, Connecticut, discussed what practitioners need to know about hemangiosarcoma to help their clients make the best decision for their pet and family.
How does hemangiosarcoma present?
According to Ettinger—known by many as Dr. Sue Cancer Vet—clinical signs of hemangiosarcoma vary greatly depending on tumor location and how advanced the disease is at diagnosis. Tumor location can vary from the skin to subcutaneous tissue to visceral organs. The most common primary visceral sites are the spleen, heart, and liver. As a cancer of blood vessels, hemangiosarcoma metastasizes quickly, with the liver and lungs being the most common targets.
Some patients with splenic hemangiosarcoma present with nonspecific signs such as decreased appetite, lethargy, or gastrointestinal distress; others present in hypovolemic shock after an acute collapse. Still, other patients have no clinical signs, and the mass is found incidentally.
Ettinger reminded clinicians that while large-breed dogs are generally thought to be at increased risk, any dog can present with hemangiosarcoma. German shepherds and golden and Labrador retrievers are believed to be at the highest risk, and a genetic predisposition is suspected.
The double two-thirds rule
Ettinger said that only about 45% of splenic masses are hemangiosarcoma based on the “double two-thirds rule.” According to this rule, two-thirds of patients presenting with a splenic mass have a malignant tumor. Of these malignancies, two-thirds are hemangiosarcoma. This rule is supported by the literature, which shows 45% to 65% of splenic masses in dogs to be hemangiosarcoma.1,2
Differentials for the one-third of dogs with benign masses include nonneoplastic masses
such as hematomas, abscesses, nodular hyperplasia, or a benign hemangioma. Differentials for the remaining malignancies can include lymphoma, histiocytic sarcoma, and osteosarcoma, among others.
Despite the double two-thirds rule, Ettinger said that in her experience, emergency clinicians have a higher suspicion of hemangiosarcoma when a splenic mass is identified. This is likely because patients presenting with a splenic mass in the emergency setting often have ruptured tumors and hemoabdomen, both of which increase the index of suspicion for malignancy. In 1 study that evaluated dogs presenting with nontraumatic hemoabdomen, 80% of the splenic masses were neoplastic and, of those, 88% were found to be hemangiosarcoma.3
Another exception to the two-thirds rule is that nonruptured splenic masses found incidentally, commonly called “incidentalomas,” are less likely to be malignant. In a 2016 study, only 30% of these masses were malignant.4
This incidental splenic mass found in a dog turned out to be myxosarcoma.
Preoperative diagnostics
Although the definitive diagnosis of any splenic mass is made via histopathology, clinicians should perform several diagnostics before surgery to assess patient risk and stability. Bloodwork is an essential part of the preoperative workup, including a complete blood count (CBC) and chemistry panel at a minimum. CBC results may raise the suspicion of malignancy if anemia, nucleated red blood cells, abnormal red blood cell morphology, or thrombocytopenia is present. CBC results can also help to assess perioperative mortality risk. Patients with marked preoperative thrombocytopenia or anemia (hematocrit < 30%) are at increased risk for death.5
Assess coagulation status with a prothrombin time or partial thromboplastin time, conducted in house if possible. If this test is not available in house, evaluate buccal mucosal bleeding time or clip the toenail to assess clotting. Half of the patients with hemangiosarcoma will present with a coagulopathy.
Perform chest radiographs prior to surgery to assess for gross meta- static disease, which is present in 50% of dogs at the time of diagnosis. Obtaining 3 views of the chest is essential to maximize the chances of detecting a lung nodule if present.
If available, abdominal ultrasonography can be a helpful tool because it is less affected by effusion than radiographs. Ultrasonography allows the clinician to confirm the presence of splenic tumor(s), assess the degree of effusion, and assess for gross metastasis to other abdominal organs. Additionally, it can help evaluate the architecture of the mass, which guides the decision to perform a fine-needle aspiration (FNA). FNAs are not recommended on cavitated splenic masses. Generally, cytology is low yield and inaccurate for hemangiosarcoma, and obtaining the sample carries a high risk for hemorrhage due to the friable nature of the mass. If a solid splenic mass is visualized, an aspirate may aid in the diagnosis.
It is impossible to distinguish benign vs malignant masses based on abdominal ultrasound alone. The splenic mass seen in this ultrasound image was determined to be hemangiosarcoma.

While some textbooks recommend echocardiography before surgery to screen for right atrial masses, Ettinger does not feel it is necessary in most cases. A better use of the client’s money is electrocardiographic monitoring during and after surgery, as arrhythmias are common in patients with both benign and malignant masses. The presence of intraoperative ventricular arrhythmias doubles the risk of perioperative mortality.5
Traditional treatment options
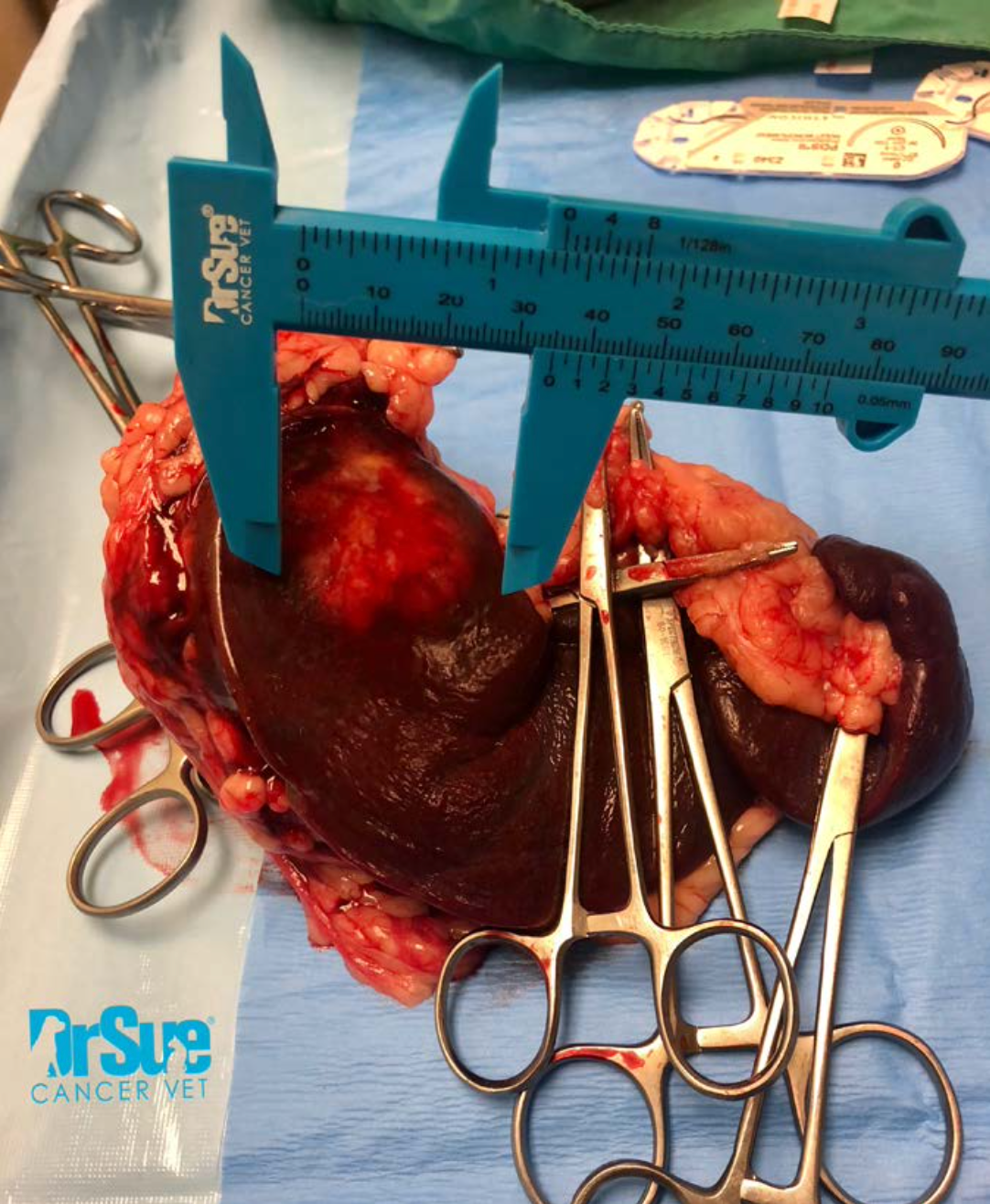
Hemangiosarcoma is a treatable cancer and treated dogs do live longer. However, the 1-year survival is less than 10% regardless of how aggressive treatment is.6 Nonruptured and low-grade splenic tumors offer the best prognosis. Surgery is the firstline treatment for splenic masses. During surgery, fully explore the abdomen. The gross appearance and size of the primary mass at the time of surgery do not correlate with malignancy. Suspected meta- static lesions on other abdominal organs, such as the liver, may be hematomas, extramedullary hematopoiesis, or another benign process. Thus, biopsy and submit all suspicious lesions for histopathology along with the entire spleen. Surgeons must remember that hemangiosarcoma can only be diagnosed definitively by histopathology and should not make intraoperative assumptions about malignancy.
Ettinger cautioned that the iatrogenic spread of neoplastic cells is possible due to the tissue’s highly friable nature. To minimize seeding of neoplastic cells during surgery, lavage the abdomen thoroughly prior to closure and use fresh gloves and instruments for closure.
Surgery alone is considered a palliative treatment that controls local disease and reduces acute hemorrhage risk in the future. Average survival time following palliative surgery is 1 to 3 months.7
Average survival time can be extended to 6 to 9 months when surgery is followed by systemic chemotherapy. Doxorubicin-based protocols are the most common, but the accumulated cardiotoxicity limits the number of treatments a patient can receive. Other protocols, including the use of metronomic chemotherapy, are being investigated to maximize survival times and quality of life following surgery.
There is also ongoing research into new therapeutic options for hemangiosarcoma, but limited data are available at this time. A new drug called eBAT is being studied at the University of Minnesota as both a treatment and preventive option. Losartan, an angiotensin II blocker in dogs, is being investigated as a possible palliative option due to its antitumor effects. Ettinger said she is excited about the potential of new therapies, but more research is needed.
The role of supplements
Ettinger also discussed the use of supplements as a part of both palliative and curative-intent treatment protocols. Polysaccharopeptide mushrooms are an Asian blend of mushrooms that have antitumor properties. Several blends are available, but many are proprietary, which makes comparing brands difficult. Ettinger recommends I’m-Yunity, which was used in a small study of 15 dogs and showed a slight increase in survival times beyond surgery alone.8 However, this product can be expensive, so she offers an alternative, K9 Immunity Plus (K9 Medicinals), noting that this blend has not been studied.
Yunnan Baiyao, a Chinese herbal mixture commonly used in veterinary patients with hemorrhage, may also help patients with hemangiosarcoma. Ettinger suggests this product as a palliative measure for patients with metastatic nodules that could rupture and bleed or in cases of splenic tumor that has ruptured, but the client declines surgery.
Key talking points for clients
When talking to clients about hemangiosarcoma, Ettinger suggests describing it as an “aggressive and malignant cancer of blood vessels” that can occur in many locations in the body. She stresses to clients that noninvasive tests will not tell us if a splenic mass is hemangiosarcoma. Wait for biopsy results before giving an accurate diagnosis and prognosis. Treatment for hemangiosarcoma is fought on 2 fronts: locally (where the cancer is growing), and distantly (where the goal is to control metastatic disease). According to Ettinger, despite the poor long-term prognosis, many of the clients she treats are very happy with surgery alone because the quality of life they get is good.
Kate Boatright, VMD, a 2013 graduate of the University of Pennsylvania, is an associate veterinarian and free- lance speaker and author in western Pennsylvania. She is actively involved in organized veterinary medicine at the local, state, and national levels and is a former national officer of the Veterinary Business Management Association.
References
- Eberle N, von Babo V, Nolte I, Baumgärtner W, Betz D. Splenic masses in dogs. Part 1: epidemi- ologic, clinical characteristics as well as histopathologic diagnosis in 249 cases (2000-2011). Tierarztl Prax Ausg K Kleintiere Heimtiere. 2012;40(4):250-260.
- Johnson KA, Powers BE, Withrow SJ, Sheetz MJ, Curtis CR, Wrigley RH. Splenomegaly in dogs. Predictors of neoplasia and survival after splenec- tomy. J Vet Intern Med. 1989;3(3):160-166. doi:10.1111/j.1939-1676.1989.tb03092.x
- Pintar J, Breitschwerdt EB, Hardie EM, Spaulding KA. Acute nontrau- matic hemoabdomen in the dog: a retrospective analysis of 39 cases (1987-2001). J Am Anim Hosp Assoc. 2003;39(6):518-522. doi:10.5326/0390518
- Cleveland MJ, Casale S. Incidence
of malignancy and outcomes for dogs undergoing splenectomy for incidentally detected nonruptured splenic nodules of masses: 105 cases (2009-2013). J Am Vet Med Assoc. 2016;248(11):1267-1273. doi:10.2460/ javma.248.11.1267 - Wendelburg KM, O’Toole TE, McCobb E, Price LL, Lyons JA, Berg J. Risk factors for perioper- ative death in dogs undergoing splenectomy for splenic masses: 539 cases (2001-2012). J Am Vet Med Assoc. 2014;245(12):1382-1390. doi:10.2460/javma.245.12.1382
- Helfand LC. Canine hemangio- sarcoma: a tumor of contem- porary interest. Cancer Ther. 2008;6(2):457-462.
- Mullin C, Clifford CA. Hemangiosarcoma. In: Small Animal Clinical Oncology. 6th ed. Elsevier Saunders; 2020:773-778.
- Cimino Brown D, Reetz J. Single agent polysaccharopeptide delays metastases and improves survival in naturally occurring hemangio- sarcoma. Evid Based Complement Alternat Med. 2012;2012:384301. doi:10.1155/2012/384301
