The first 3 minutes: Recognizing a horse in shock
With a stepwise triage exam, you can quickly recognize an equine patient in shock. Your clinical impressions and understanding of the cardiovascular circuit can help identify the type of shock, which will guide your treatment plan.
When you first approach a horse that may be in shock, “You're asking yourself, ‘Is this patient cardiovascularly stable? Do I need to do something to keep it alive until I can figure out what's going on?'” says Jarred Williams, DVM, PhD, DACVS, DACVECC, a clinical assistant professor in Large Animal Emergency Medicine at the University of Georgia College of Veterinary Medicine. In his recent Fetch dvm360 conference session, Dr. Williams shared his strategy for identifying a horse in shock and ways to differentiate the types of shock, based on where the problem is in the horse's cardiovascular circuit.
The definition of shock
When a horse is in shock, the bottom line is that its tissues are not being perfused adequately. Dr. Williams says, “The important thing about blood not getting where it needs to go is that red cells saturated with oxygen are also not getting there.” Although cells can survive without oxygen for some time through anaerobic metabolism, it comes down to the balance between how much ATP the cell is making versus how much ATP the cell is using. Dr. Williams says, “Technically speaking, shock is all about the ATP.” But he acknowledges that you can't say to clients, “I don't think your horse's cells are producing enough ATP.” Instead, you can say, “I don't think blood flow is going where it needs to well enough.”
Dr. Williams explains, when oxygen is available, that a cell can make a ton of ATP, but without oxygen it can only make a little bit (32 to 36 ATP with aerobic metabolism versus approximately 4 ATP with anaerobic metabolism-remember studying the Krebs cycle in biochemistry class?). In a sick animal, you might have decreased oxygen delivery (DO2). The horse might be dull, depressed, barely moving, so its oxygen utilization (VO2) is also reduced.
What's important is the ratio between DO2 and VO2, Dr. Williams says.
“It's like your bank account-it doesn't really matter how much money you make,” he says. “It's how much money is in your account at the end of the month. If you make $1 million a month, but spend $2 million a month, you're going to be in the red quick. If you make $10, but don't spend any of it, you're going to stay in the black. All we really care about is that the DO2 stays above the VO2 in any scenario. If that happens, you're normolactemic and likely perfusing adequately.
“The bottom line is when you're not perfusing adequately, then your VO2 can exceed your DO2, and your cell needs may not being met,” Dr. Williams says. “That's a state that you cannot survive for a prolonged period.”
The 3-minute triage examination
Dr. Williams says that when you perform your initial triage examination of a sick patient, you're figuring out whether the horse is unstable and, if so, how you're going to stabilize it (Figure 1). When a horse is not cardiovascularly stable, it needs to be stabilized before you can proceed with any other treatment. You need to quickly determine why it's unstable, so you can determine the best way to stabilize it.
Figure 1
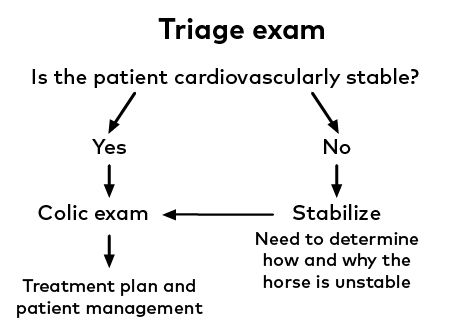
“Some treatments for shock would be the exact opposite treatment for other types of shock,” Dr. Williams says. “So, knowing what type of shock has occurred is vital.” Once the horse is stabilized, you can proceed and figure out what's actually occurring with the horse to put it in that state in the first place.
Dr. Williams says one of the most helpful parts of the triage examination is looking at the horse's mentation: “When the horse walks through the door, does it seem mentally appropriate? Is it dull or depressed? Does it seem ataxic because of a primary neurologic problem, or is it ataxic out of weakness? Watching the horse walk in and seeing its demeanor, trying to extrapolate about blood flow to the brain is important.”
Dr. Williams says that veterinarians may have learned to do their triage examinations differently, but he always starts at the head: “I feel the ears and assess the horse's peripheral temperature in relation to its core. I look at the eyes-are they sunken? I look at the gums, pick up the lips, check the capillary refill time (CRT). I feel under the horse's face for a pulse. I'll check the jugular refill time and listen to the heart for any arrhythmias. Does it sound muffled? Then I'll work my way further down. I'll feel the distal limbs for coolness. I typically listen to the GI tract because I'm right there, even though that's not really part of a triage exam. Then I listen to the lungs and take a core temperature.”
Identifying where the problem lies in the circuit
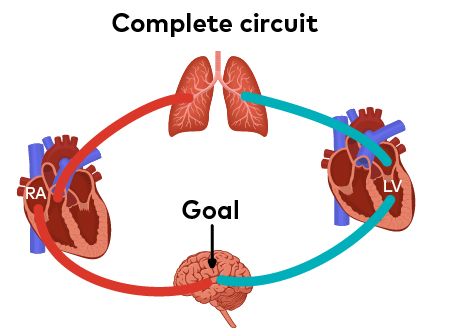
As you know from anatomy classes, the cardiovascular system creates a closed circuit (Figure 2). The blood leaves the right heart, goes to the lungs, picks up oxygen and goes back to the left heart. The left heart's whole job is to send oxygenated blood to the tissues. After the oxygen is delivered, the deoxygenated blood goes back to the heart. Dr. Williams says, with the different types of shock, there's a problem somewhere in this circuit-either with the pump, the tubing or the fluid.
Figure 2
The pump
“Everything starts with the heart because that's the pump,” says Dr. Williams. However, there's not that much the heart can do to help perfusion. It can speed up or slow down; it can beat harder or slower (contractility); and it can help contribute to the amount of volume that comes out of it.
“That's all the heart can control,” he says. “The heart is beholden to the volume that's coming to it and the pressure it is beating against. The main aspects the heart can control are rate and contractility.”
The amount of blood that leaves the heart with one beat is the stroke volume. Cardiac output is how much blood leaves the heart in 1 minute. A normal horse's cardiac output is 32 to 40 liters/minute.
“That's an insane volume going through in a minute-insane!” Dr. Williams says. “That's a testament to how big the equine heart is.” And, if 32 to 40 liters are leaving the heart every minute, that means 32 to 40 liters are being delivered to the tissues every minute, as long as the circuit is closed.
There are three things that determine stroke volume (how much blood leaves the heart with each beat)-preload, afterload and contractility.
Preload is how much volume is coming into the heart. “You may not consciously think that you're giving intravenous fluids because you want to affect preload, but that is what you're doing-increasing the volume of fluid coming to the heart,” says Dr. Williams.
Afterload is the pressure against which the heart is beating. “Don't view it as a load or volume that's coming back after the beat,” he says. “Think about it as the pressure against which the heart is beating. It's not truly a pressure, but decreasing afterload means that the heart can pump blood more easily. Increasing afterload means the heart is pumping against something and it's more difficult for blood to leave the heart.” Less blood is going to leave the heart the more constricted large arteries after the heart are. Drugs that cause dilation can help reduce afterload.
Contractility is how hard the heart is beating, which can be increased or decreased. “When I exercise and feel my heart beating through my chest, that's my body trying to increase stroke volume, so it can increase cardiac output, so I deliver oxygen better,” says Dr. Williams.
The tubing
“Shock is not just about the heart,” says Dr. Williams, “and actually, in horses, it's rarely about the heart. We infrequently have cardiac problems in horses.” So, if it's not the pump, you could have an issue with the tubing, he says.
There can be any sort of dysfunction in the arteries, which have muscular control and can constrict and dilate, and in the veins. If the blood vessels aren't doing their job, blood will only be delivered as far as the heart can pump it. “So you have pressure that leaves the heart and then tubing that takes the blood where it needs to be,” Dr. Williams explains.
The fluid
There can also be a fluid issue. “The vast majority of shocky animals you see are going to have hypovolemia, a loss of volume,” he says. “A loss of volume equals decreased stroke volume-decreased stroke volume because of decreased preload and decreased perfusion.”
Occasionally there's adequate delivery of oxygen to the cells but the cells aren't functioning correctly. Dr. Williams says that happens now and then with certain endotoxemia problems or ischemia-reperfusion injury leading to cellular dysfunction or “metabolic problems.”
Now, back to the triage exam: “With your triage exam, you're really just asking, ‘Where on this circuit is the problem?'” There is a hierarchy of tissues needing perfusion: the most important are the brain, heart, and lungs; next is the kidneys; then the gastrointestinal tract and enterohepatic system; and then the periphery.
“It would make no sense to have abnormalities in your cardiovascular circuit and not try to steal blood from an area that doesn't matter as much,” he says. “So, cold periphery, delayed CRT, that's telling you that you might have an issue with circulation to places that matter.”
The types of shock
Dr. Williams says that if you understand the circuit, it's easy to remember the types of shock: distributive, hypovolemic, obstructive, cardiogenic and metabolic/hypoxic.
Distributive shock is a tubing problem. “If the muscles in the arteries don't constrict and dilate, blood is pumping into an open, floppy bag of a vessel,” he says. “The blood is only going to go as far as the heart can pump it.” This sort of shock occurs in cases of sepsis and SIRS (systemic inflammatory response syndrome) and in severe hypotensive patients.
Hypovolemic shock is a fluid problem. There's not enough volume in the tubing. It's the most common type of shock, and it can occur with dehydration. With hemorrhagic hypovolemia, there's an open circuit, and the patient is losing blood somewhere.
Obstructive shock occurs when the circuit is obstructed in some way. The obstruction can be intravascular or extravascular.
“You could have an obstruction within the vessels, a massive occlusion in a major vessel-like the vena cava,” he says. The circuit stops because of this intravascular obstruction.
An example of an extravascular obstruction is a colon that is enlarged by gas that pushes the abdominal wall out: “If you do a rectal exam, the colon is pushed back in the pelvic inlet. It pushes against the diaphragm and the patient has difficulty breathing. With enough pressure, the vena cava may be occluded, which decreases the return to the heart. Preload will drop, and you will have obstructive shock,” he explains. In dogs, this would be a gastric dilatation volvulus. Dr. Williams says that in horses you can see this with some pregnancies or with ascites.
Cardiogenic shock is a pump problem. This occurs mainly with congestive heart failure or a heart attack.
Metabolic or hypoxic shock is an oxygen problem. There are two forms of hypoxic shock-hypoxemic and cytopathic. With hypoxemic shock, desaturated blood failing to becoming saturated for some reason-whether that's because of lung disease, altitude or shunting. “Everything is circulating just fine, but the body is delivering red cells that aren't carrying much oxygen,” says Dr. Williams.
In cases of cytopathic shock, there is cellular dysfunction: “This is the worst because the triage exam is going to look relatively normal,” he says. “They're not hypovolemic. The tubing is fine, and the heart is working. They're doing everything right. They're delivering the oxygen to the cell, but the cell is not working. That's a horrible problem to have.”
This happens with ischemia-reperfusion injury. “You cut off blood supply, protein gets denatured, and cell walls get broken,” he says. “Then when you get blood flow back, the cell doesn't know what to do with it because the organelles, the parts of the cell that are supposed to handle the oxygen, are broken.”
Still, in all scenarios, regardless of why you have poor perfusion, the relationship between DO2 and VO2 is the key. “In equine patients, the DO2 is almost always lower than VO2 because of poor oxygen delivery,” he says. “It's not usually because of increased oxygen utilization, at least not in sick patients.”
Sick animals try to decrease VO2 by not moving, Dr. Williams says: “That's why animals with colitis, enteritis or pneumonia are lethargic and look like they do. They don't have energy. But when we say they don't have energy, what we mean is they're doing everything they can to send oxygenated blood to the vital organs to stay alive. That's why the exam shows cold extremities and abnormal mucous membranes.”
Measuring lactate concentration
Dr. Jarred Williams' advice? Carry a lactometer.
Dr. Williams knows that many practitioners can recognize when a horse is in shock without using a lactometer. However, using a lactometer allows you to quantify your assessment. (And it is, incidentally, a good way to capture fees, he says.)
“What's difficult is that sometimes the cardiovascular compensation for decreased stroke volume or decreased cardiac output-the increased heart rate-is sufficient,” he says. “The animal might be persistently tachycardic, not because of pain, but because that's its compensation. And you might be fooled and think it doesn't look like it's in shock.”
Dr. Williams believes that lactate concentration is one of the more valuable pieces of bloodwork: “As far as the quick, ‘Can I take a deep breath on this case?' or ‘OMG, we need to do more!' … lactate helps me more than anything outside of the physical examination.”
One way to confirm that a horse is not perfusing tissues adequately (is in shock) is to determine whether it's hyperlactatemic. (Normal lactate concentration for a horse is less than 2 mmol/L.)
“When you're hyperlactatemic, that's the body tweeting that VO2 is higher than DO2,” Dr. Williams says. “As long as DO2 is higher than VO2, you're in aerobic metabolism, and your cell will not create lactate-it doesn't need to. However, when VO2 is higher than DO2, when you're not perfusing adequately, you will go into anaerobic metabolism.”
Lactate is a byproduct of anaerobic metabolism. Therefore, identifying hyperlactatemia signals that the anaerobic process is happening: “When you see increased lactate, the cell is demonstrating that VO2 is winning, and DO2 is losing. This could be due to decreased DO2, as in most sick patients, or it can be due to increased VO2.” (See "Dr. Jarred Williams' advice? Carry a lactometer" on this page.)
Summary
When you do your triage examination, you're quickly ascertaining, “Do I think this horse is in shock?” The answer to this question may prompt referral or point to steps needed to stabilize the horse.
“It's your quick examination that is so telling,” Dr. Williams says. “For me it's the cold periphery, the delayed CRT and the delayed jugular refill-there's not many reasons for that to happen.”
Once you recognize that shock is happening, you need to identify the type of shock. You need to know why the DO2 is decreased to know how to increase it.
In the field, treatment for shock is usually going to be fluid therapy, unless you've identified that it's a heart problem and the horse should not be given fluids. Dr. Williams advises keeping catheters and hypertonic saline solution in your practice truck.
“When you identify that a patient is in shock, and determined it's not cardiogenic, you can hang a liter of hypertonic saline solution while you're doing the rest of your examination,” he says. “That alone is going to help tremendously.”
The time it takes to get a catheter placed and fluids infusing in the first 45 minutes will allow you to tell the owners, “This is what I think is going on. We're more stable than we were an hour ago.”
Dr. Williams says you should be in a much better place to either refer the horse or move forward with diagnosis and treatment of the underlying problem.
Jarred Williams, DVM, PhD, DACVS, DACVECC, is a clinical assistant professor in Large Animal Emergency Medicine at the University of Georgia College of Veterinary Medicine. His clinical interests include surgery, gastrointestinal disease, trauma and emergency and critical care. His research interests include biomechanics.