Image Quiz: Test your diagnostic and treatment skills in these oncology cases
Veterinary patients with masses, abnormal test results and specific clinical signs point to clear diagnoses. How well would you do identifying these patients conditions?
Dog A (All images courtesy of Dr. Brooke Britton.)

Dog B

Dog C

These three dogs share the same condition, with vastly different clinical presentations. Dog A developed a rapidly growing, ulcerated and superficially infected mass on the hindlimb over the course of three weeks. Dog B developed too-numerous-to-count, intensely pruritic dermal lesions and progressive lethargy over the course of several months. Within months after surgical excision of a mass, Dog C developed painful subcutaneous lumps over the dorsum, with straining to defecate, inappetence and intermittent vomiting.
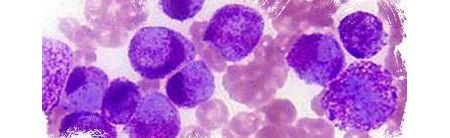
Fine-needle aspiration of the lesions was performed in each dog. The cytology in each dog was similar in appearance, shown below:
1. What's your diagnosis?
A. Mast cell tumor
B. Eosinophilic granuloma complex
C. Cutaneous plasma cell tumor
D. Atypical variant of lymphoma
The correct answer is A: mast cell tumor
The majority of canine mast cell tumors occur as solitary lesions in the dermis and subcutis, primarily over the trunk and limbs; however, 10% to 15% of dogs have multifocal disease at presentation.
Mast cell tumors exhibit a wide spectrum of phenotypes and have unpredictable biologic behavior. Many dogs are clinically well at diagnosis, but a subset will demonstrate tumor-associated signs secondary to release of tumor granule substances (i.e. histamine, heparin, other vasoactive amines). These can include localized tissue reactions (e.g. bruising, edema, ulceration, erythema, pruritis), systemic signs (e.g. inappetence, vomiting, diarrhea, fever) or both.
Spread of mast cell tumors occurs via the lymphatic system to the regional lymph nodes, abdominal viscera and, less commonly, the bone marrow; spread to the chest cavity and other bodily locations is rare. Dog C experienced tenesmus due to enlarged medial iliac lymph nodes that were compressing the colon and affecting defecation as a result.
Most canine mast cell tumors can be diagnosed readily on fine-needle aspiration and cytology. Cytology typically yields large, granulated round cells with prominent nuclei that stain intensely purple on application of Diff-Quik. Biopsy of mast cell tumors is required to provide grading and additional prognostic information.
2. What should the ideal next steps be in the workup of these dogs?
A. Complete blood cell count (CBC) with serum chemistry panel
B. Thoracic radiographs
C. Abdominal ultrasound plus or minus organ fine-needle aspiration
D. Buffy coat smear
E. A, B and C
F. All of the above
The correct answer is E: CBC, chest radiographs and abdominal ultrasound
Staging should be considered in dogs with mast cell disease regardless of presentation and is strongly recommended in all dogs with large, rapidly growing or recurrent mast cell tumors. Staging diagnostics include a minimum database (CBC with serum chemistry profile, plus or minus urinalysis), thoracic and abdominal imaging, and regional lymph node aspiration where possible. Advanced imaging may be useful in patients with large, fixed or invasive tumors.
Buffy coat smears are not considered informative in staging or monitoring of dogs with mast cell tumors, as mastocytemia is more commonly associated with non–mast-cell-related disease in dogs. In addition, random detection of mast cells in blood smears in dogs is usually not secondary to mast cell tumors.
A 10-year-old male castrated West Highland white terrier was recently evaluated by his primary veterinarian for three weeks of stranguria with occasional hematuria and increased marking behavior. He has otherwise been a healthy dog with no signs of systemic illness.
Free-catch urinalysis was remarkable for 2+ proteinuria, 2+ blood, occasional atypical cells as seen below and a urine specific gravity of 1.045. Occasional rod-shaped bacteria were seen. A seven-day course of amoxicillin/clavulanate (Clavamox-Zoetis) was prescribed empirically, with improvement of lower urinary tract signs observed within three days.

Recurrence of urinary straining and hematuria was observed two weeks after completion of the antibiotic course. Amoxicillin-clavulanate was represcribed for a 10-day course, with initial improvement followed by recurrence of urinary straining and hematuria within one week.
3. What is the next step in the management of this patient?
A. Switch to a fluoroquinolone antibiotic, prescribing a two-week course of medication.
B. Represcribe amoxicillin/clavulanate, and continue it for one month if initial improvement is seen.
C. Conduct urine culture and sensitivity testing; consider abdominal ultrasound.
D. Prescribe amoxicillin and a fluoroquinolone; continue combination therapy for at least two weeks.
The correct answer is C: Conduct urine culture and sensitivity testing; consider abdominal ultrasound.
Given the lack of durable resolution of lower urinary tract signs on initial antibiotic therapy, urine culture and sensitivity testing are indicated. In light of this patient's signalment, the index of concern for underlying urinary tract disease should be increased, and abdominal ultrasound, particularly if urine culture is negative, should be recommended.
A clean catheterized urine sample was obtained, and culture confirmed a bacterial infection with intermediate sensitivity to amoxicillin and sensitivity to fluoroquinolones. A two-week course of marbofloxacin was prescribed, with complete resolution of lower urinary tract signs within three days. The antibiotic course was completed, and within two weeks lower urinary tract signs recurred. Abdominal ultrasound was performed. Significant findings on imaging included an enlarged, irregular prostate and a masslike lesion within the urinary bladder at the level of the trigone.
4. What is the primary differential?
A. Granulomatous cystitis
B. Transitional cell carcinoma
C. Benign prostatic hyperplasia with bladder hematoma
D. Benign bladder polyp
The correct answer is B: Transitional cell carcinoma
Transitional cell carcinoma is the most common urinary bladder cancer in dogs, with an increased prevalence in small terrier breeds. Transitional cell carcinoma is typically an invasive tumor within the bladder and occurs near or at the level of the trigone in the majority of patients. Recurrent urinary tract infections are common in patients with this disease.
5. The owners of this dog are interested in minimally invasive testing to confirm the putative diagnosis and wish to avoid cystoscopy or surgery if possible. They also have cost concerns and would like to maximize the chance of obtaining a diagnosis without performing multiple different tests. What represents a highly sensitive and specific test that may accomplish this?
A. Bladder tumor antigen test
B. Direct aspiration of the bladder mass (plus or minus prostate) under ultrasound guidance
C. Cadet BRAF assay
D. Cytologic analysis on centrifuged urine sample
The correct answer is C: Cadet BRAF assay
The Cadet BRAF assay (Antech Diagnostics) is a highly specific and sensitive test used to support a diagnosis of transitional cell carcinoma or urothelial carcinoma in dogs. This assay, a noninvasive test performed on a free-catch urine sample, is capable of detecting urinary tract carcinoma months before clinical signs develop. The assay identifies tumor cells carrying a specific mutation in the canine BRAF gene, which is present in urine samples from 85% of all transitional cell/urothelial carcinoma cases. The BRAF mutation has not been detected in urine from dogs with various other forms of cancer, nor with nonmalignant bladder inflammation or polyps. The CADET assay is also not affected by the presence of blood or bacteria in the urine.
The other test options presented are reasonable to consider; however, they lack the specificity or sensitivity of the BRAF assay. The bladder tumor antigen test is sensitive but lacks adequate specificity as false positives are common with concurrent bladder inflammation and infection. Direct aspiration of the bladder mass presents a risk of tumor seeding within the abdomen. Spun cytology of urine may in some cases support a diagnosis of carcinoma; however, epithelial atypia can occur secondary to bladder inflammation and urinary tract infection, which may confound interpretation of centrifuged urine samples.
6. The Cadet assay was performed and was positive, consistent with a diagnosis of bladder carcinoma. Therapeutic options for this disease include:
A. Surgery
B. Radiation therapy
C. Chemotherapy
D. NSAID therapy
E. All of the above
The correct answer is E: All of the above
Options for treatment include nonsteroidal anti-inflammatory drugs (NSAIDs), surgery, chemotherapy and radiation therapy. Additionally, for tumors that are obstructing the ureters, urethra or colon, stents can be placed to help keep these passageways open. Due to the invasive nature of these tumors, surgical cure is not typically possible. Regrowth is very common after surgery due to microscopic seeding of the tumor within the bladder lining, even when a “complete” excision is apparently achieved on histopathology. Apical tumors are typically better candidates for surgical cytoreduction compared with tumors located within or encroaching on the trigone.
Blocking the COX-2 enzyme in cancer cells with NSAIDs is thought to play a role in slowing tumor growth as well as in decreasing any tumor-associated inflammation. The majority of dogs treated with NSAID therapy experience improvement in their lower urinary tract signs, and approximately 20% of patients experience objective (often partial) tumor shrinkage with therapy.
Chemotherapy as well as oral anti-tumor medications, such as toceranib phosphate (Palladia-Zoetis), can impair growth of the primary bladder tumor and progression of metastatic disease. Radiation therapy can also be used in the treatment of transitional cell carcinoma to treat the primary tumor in place of surgery, to treat residual disease within the bladder postoperatively, for relief of pain associated with bony metastases, or to slow the growth of enlarged metastatic lymph nodes. The addition of radiation therapy to surgery, chemotherapy and NSAID treatment may improve outcomes in a subset of patients with this disease.
The prognosis for patients with transitional cell carcinoma depends on the extent of cancer involvement at diagnosis, with cancers that have metastasized or involve the urethra having worse prognoses than those localized within the bladder. Without treatment, most dogs will die within months as a result of complications of their disease. With chemotherapy, the median survival time approaches 1 to 1.5 years in dogs with bladder involvement, and six months if there is urethral (or, in males, prostatic) involvement. Unfortunately, treatment is rarely curative and therefore focused on maintaining comfort and a good quality of life.
Dr. Brooke Britton is with BluePearl Specialty and Emergency Pet Hospital in New York City.
