Measuring blood pressure and managing hypotension in the surgical patient
During anesthesia, trends in blood pressure must be monitored to develop a protocol and manage hypotension.
Hypotension is one of the most common intraoperative complications seen in small animals under anesthesia. A variety of injectable and inhalant anesthetic drugs can cause varying degrees of hypotension triggered by numerous factors including heart rate, preload, afterload, contractility, and systemic vascular resistance. Hypotension can lead to decreased perfusion in vital organs (eg, liver, kidneys, heart), which leads to reduced oxygen delivery. Veterinary technicians working with patients under anesthesia need to understand how to measure blood pressure, the factors that lead to hypotension, and how to properly address hypotension in these patients.
Measuring blood pressure
Palpating pulses in the anesthetized patient is essential. However, simply palpating a pulse is not a strong indicator of adequate blood pressure. When you are feeling pulse pressure, you are thought to be sensing the difference between systole and diastole. However, when anesthetic agents are on board, especially agents that cause vasoconstriction, you may feel a decreased pulse pressure despite normal blood pressure readings. Therefore, merely feeling a pulse should not be used as a barometer of your patients’ blood pressure.
There are 3 ways to measure blood pressure in patients are under anesthesia.
Direct vs indirect measurement
Direct arterial blood pressure measurement involves arterial catheter placement and continuous readings via a pressure transducer. An appropriately sized catheter is inserted into an artery such as the dorsal pedal artery. Arterial cannulation of an artery can take a bit of skill because the tunica media in the arteries contains smooth muscle cells and elastic tissue, thicker than that in veins. Once a catheter is secured properly into an artery, this measurement is easier to perform than you might think (Figures 1-3).
Figure 1. Basic setup for placement and monitoring of arterial blood pressure. From left to right: pressure bag for sodium chloride (NaCl), heparinized NaCl bag, heparin 1000 U/mL, fluid bag spike and transducer appropriate for your multiparameter monitor, appropriate-sized catheter, T set flushed with heparinized saline, extra heparinized saline flush, medical tape to secure catheter.
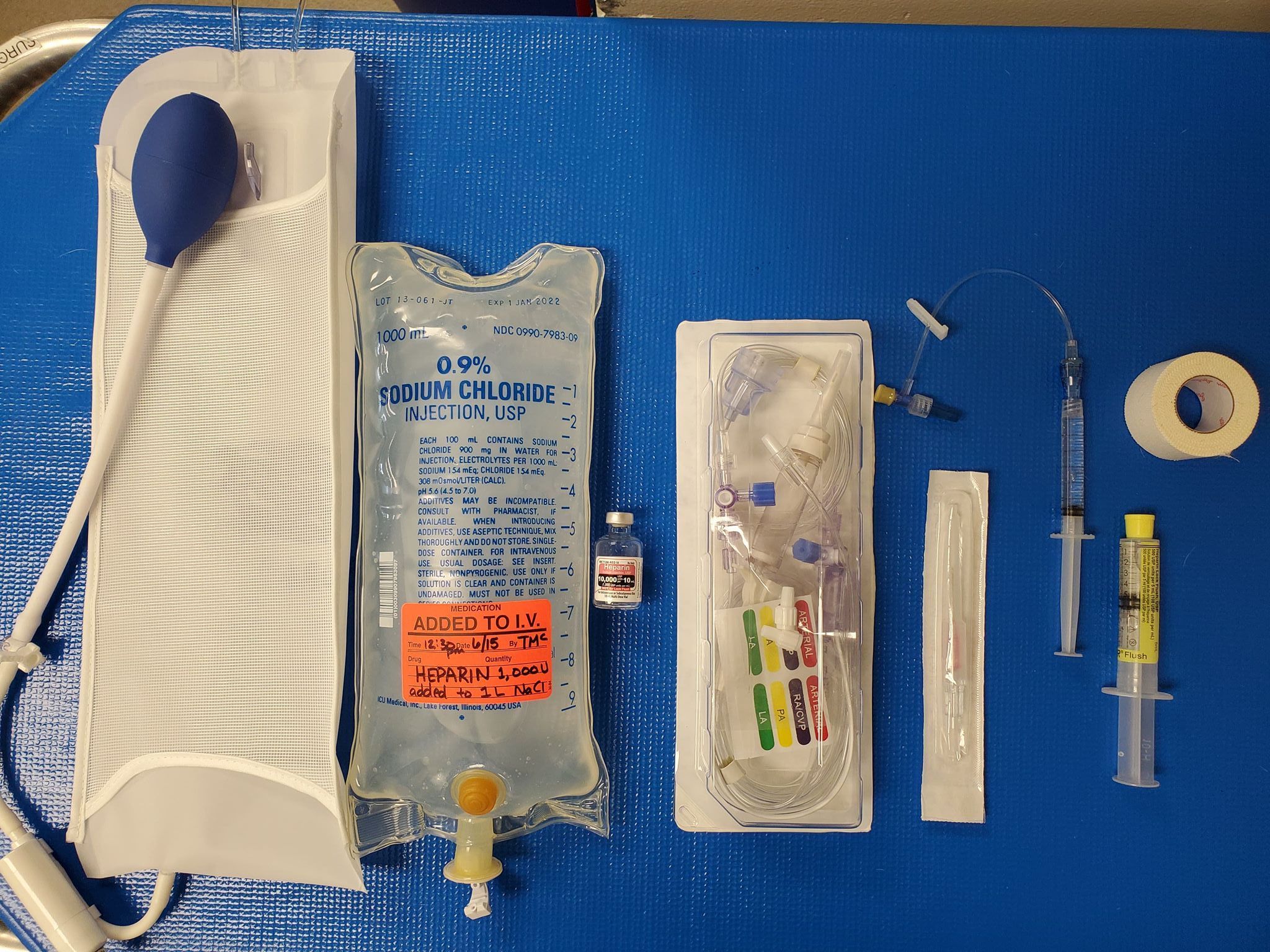
Figure 2. Placement of catheter into the dorsal pedal artery.

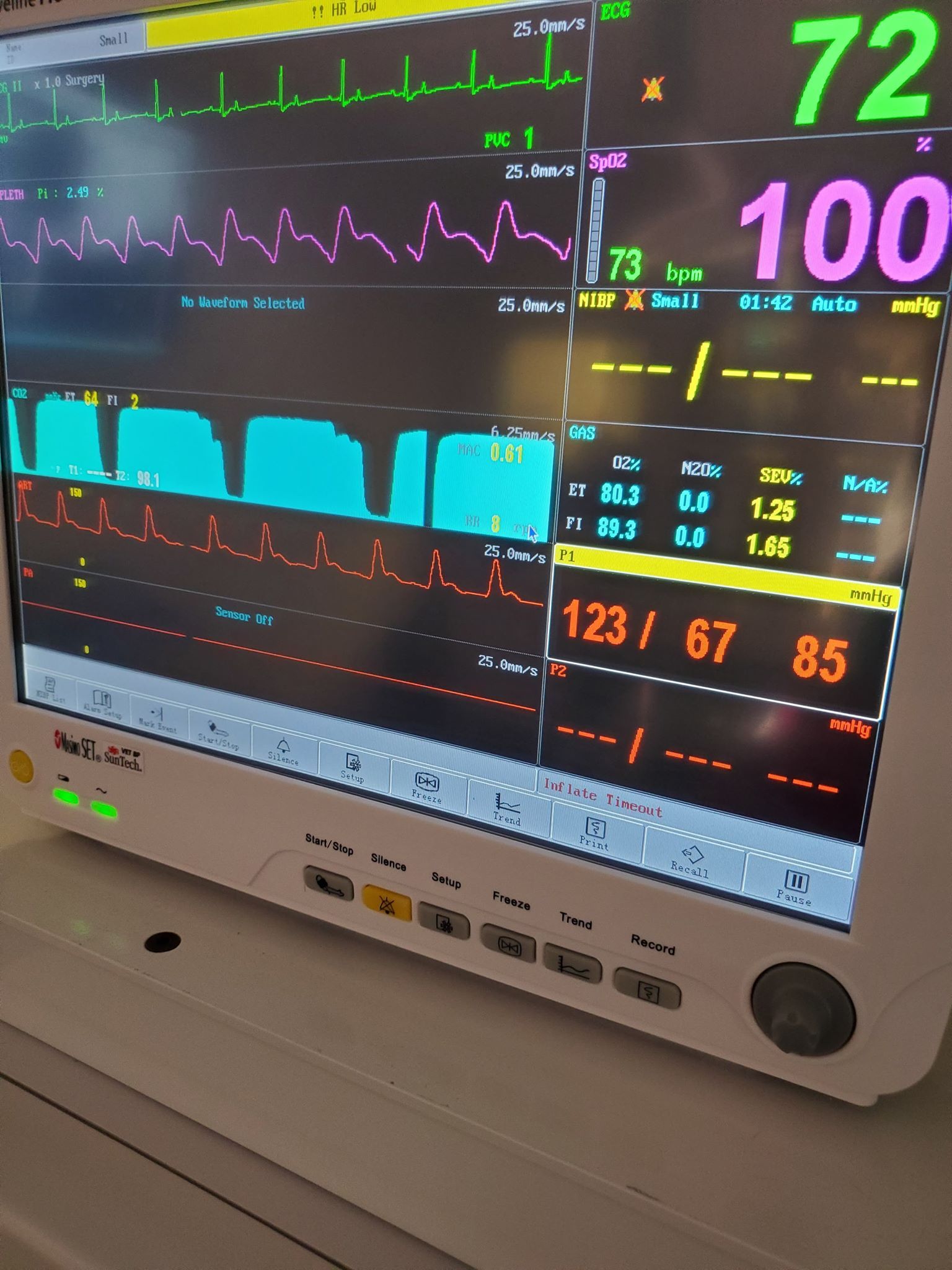
Figure 3. Direct arterial pressure waveform shown during a surgical procedure.
Critical patients undergoing surgery should be considered for this method, which is beneficial in the following scenarios:
- Patients that are hypovolemic due to trauma or hemoabdomen
- Patients with pre-existing cardiovascular disease (eg, severe dilated cardiomyopathy)
- Patients undergoing procedures in which significant blood loss or large fluctuations in blood pressure are anticipated (eg, surgery in patients with pheochromocytoma)
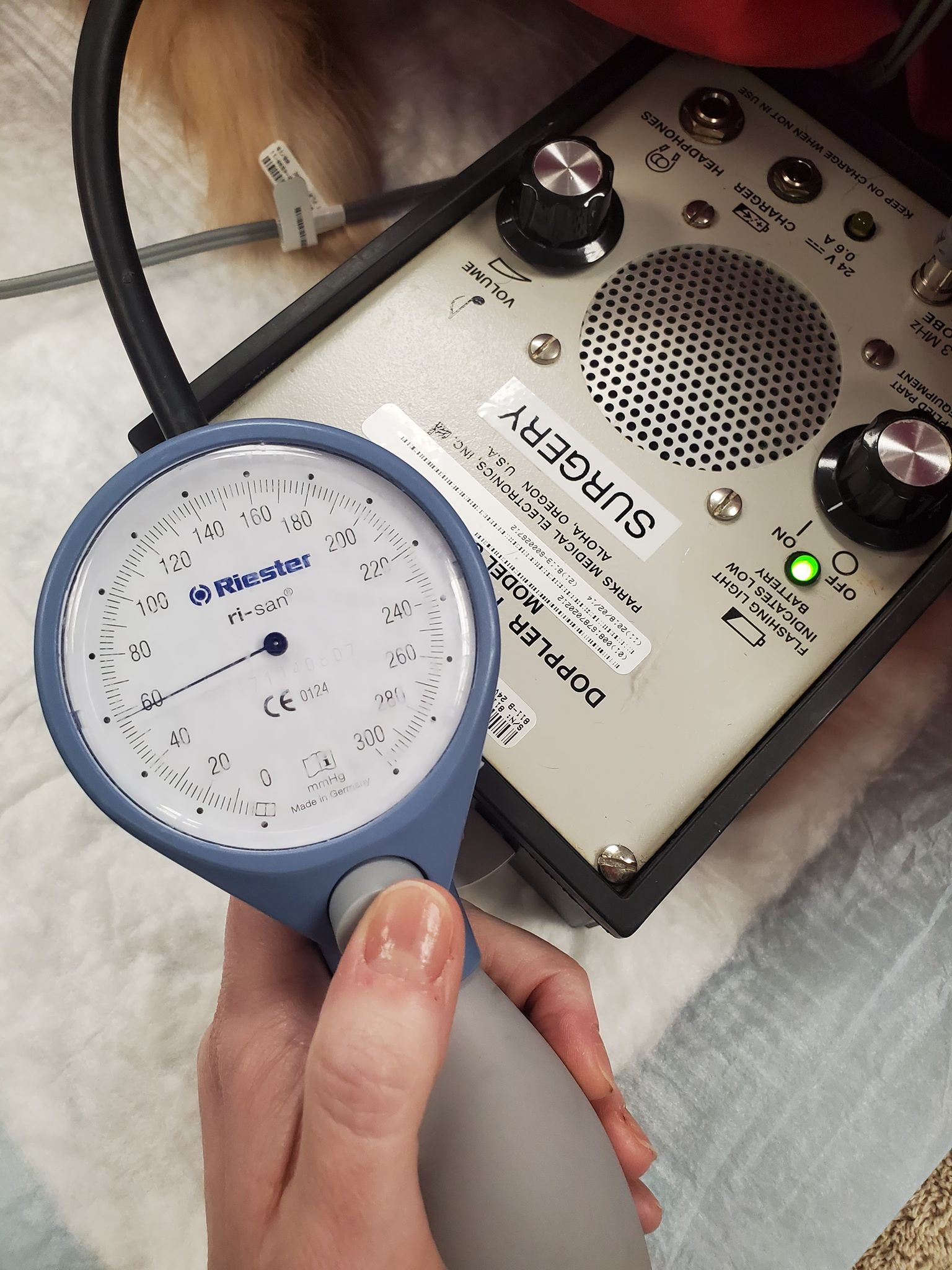
Indirect methods of measuring blood pressure, such as Doppler ultrasonography and oscillometric measurement, are used more frequently in small animal practices than is direct arterial placement. Doppler ultrasonography blood pressure measurement (Figure 4) using a sphygmomanometer is preferred in cats and small dogs (< 10 kg [~22 lb]). Oscillometric measurement involves use of equipment that automatically inflates and deflates a cuff to determine blood pressure continuously. This is probably the easiest of all the blood pressure monitoring options.
Figure 4. The noninvasive Doppler blood pressure method is a good way to monitor overall trends during anesthesia and treatment.
Some veterinary practices may be intimidated by the cost of equipment needed to measure blood pressure via direct arterial catheter placement. However, the equipment required to determine mean arterial pressure alone is inexpensive compared with equipment for indirect oscillometric measurement. In addition, arterial catheters can be used to collect samples for blood gas analysis, which can provide valuable information, especially in patients with respiratory compromise.
Blood pressure cuffs
Regardless of which method you choose, keep in mind that a single reading is not used to determine treatment; instead, we look at trends in blood pressure readings. Also, remember that the placement of the cuff is important. The most consistent cuff location in small patients is mid-forelimb.
For the purpose of this article, I will apply a mean arterial pressure of under 60 mm Hg to determine hypotension. If using a Doppler method, I will apply any readings of under 100 mm Hg systolic arterial pressure to describe hypotension.
Once a hypotensive trend has been identified, the next step is to work with the veterinarian to determine a course of action for correction.
Treating hypotension
There are several ways to treat hypotension once the underlying cause has been identified. First, it is important to record each patient’s preoperative heart rate to establish an average (base) resting rate for that individual. If your patient is bradycardic and hypotensive because of a decrease in heart rate, consider an intraoperative intravenous dose of glycopyrrolate (0.01 mg/kg) until the heart rate returns to an acceptable range. On the other hand, if your patient is bradycardic and hypotensive because of administration of an α2-adrenergic receptor agonist (commonly called an α-agonist), such as dexmedetomidine, consider administering a reversal drug, such as atipamezole (0.10-0.30 mg/kg IM). If your patient is hypotensive due to the vasodilating effects of anesthetic inhalant agents, consider decreasing the dose of the agents.
Inhalant anesthetic agents can also cause a decrease in cardiac output and, when combined with vasodilation, may lead to decreased organ perfusion. Increased circulating volume can be achieved by administering boluses (5-10 mL/kg) of intravenous crystalloid fluids, which will help if hypotension is secondary to hypovolemia and peripheral vasoconstriction. In some patients, reducing anesthetic depth and administering an increased volume of crystalloid fluids is not enough to correct hypotension. In these cases, the addition of colloids or inotropic agents should be considered. Colloidal solutions can be either natural (eg, albumin) or synthetic (eg, dextran, hydroxyethyl starch). Patients that do not respond to these treatments will need intervention with drugs to improve systemic vascular resistance and contractility. These drugs act on α- and β-adrenergic receptors. Stimulation of these receptors can have varying effects at varying doses.
Of course, before starting any therapy, talk with your clinician to verify both the drug and the dose.
Dobutamine
Dobutamine is a synthetic catecholamine that acts on α- and β-adrenergic receptors, stimulating cardiac contractility, cardiac output, and coronary blood flow. Low doses can cause an increase in cardiac output while simultaneously initiating a moderate increase in heart rate. The therapeutic dose ranges from 2 to 20 µg/kg/min.1
Dopamine
Dopamine is a short-acting norepinephrine precursor with α- and β-agonist properties (ie, binds to α1-, α2-,and β2-receptors plus 2 dopamine receptors). The dosing schedule is important with this drug, as different doses can stimulate other receptors and thus trigger different effects. Medium doses (eg, 3-5 µg/kg/min) can stimulate β-adrenergic receptors that act as a positive inotrope and increase heart rate.1 Higher doses (6 to 10 µg/kg/min) stimulate α-adrenergic receptors that cause an increase in systemic vascular resistance. Doses higher than 10 µg/kg/min can trigger tachycardia and increased afterload, leading to decreased cardiac output.1
Ephedrine
Ephedrine is a noncatecholamine sympathomimetic agonist that stimulates α- and β-adrenergic receptors. Another benefit of ephedrine is improved oxygen delivery to tissues via increased hemoglobin. Ephedrine can also be administered as a single-bolus intravenous injection of 0.10 mg/kg.2
Norepinephrine
Norepinephrine acts on α- and β-receptors by increasing mean arterial pressure and peripheral vascular resistance. Coronary blood flow also increases. Norepinephrine may be beneficial in increasing mean arterial pressure in patients with sepsis or patients currently on β-blocking drugs such as atenolol.1 Often, norepinephrine infusions are started at 0.10 to 0.20 µg/kg/min and can be increased by increments of 0.10 to 0.20 µg/kg/min as needed. It is important to note that norepinephrine is not usually the first choice for hypotensive patients that are otherwise healthy. It is often used in the treatment of vasodilatory shock and commonly administered with an inotrope (such as dobutamine) if myocardial depression is suspected.
References
- Mazzaferro E, Wagner A. Hypotension during anesthesia in dogs and cats: recognition, causes, and treatment. Compend Contin Edu Pract Vet. 2001;23(8):728-737.
- Wagner AE, Dunlop CI, Chapman PL. Effects of ephedrine on cardiovascular function and oxygen delivery in isoflurane-anesthetized dogs. Am J Vet Res. 1993;54(11):1917-1922.
Tasha McNerney, BS, CVT, VTS (anesthesia and analgesia), CVPP, is an author, lecturer, and administrator for Veterinary Anesthesia Nerds.
