WVC 2017: Probiotics - Not Just for People Anymore
At the 2017 Western Veterinary Conference in Las Vegas, Stanley Marks, BVSc, PhD, DACVIM, DACVN, discussed what we know—and more of what we’ve yet to discover— about microbial gastrointestinal health.

Interest in medicinal nutrition continues to grow. At the 2017 Western Veterinary Conference in Las Vegas, Stanley Marks, BVSc, PhD, DACVIM (Small Animal Medicine and Oncology), DACVN, discussed what we know—and more of what we’ve yet to discover— about microbial gastrointestinal (GI) health.
The term “microbiota” refers to the population of microbes that inhabit body ecosystems. The average human digestive tract contains an estimated 100 trillion bacteria—10 times the number of cells found in the body.1
RELATED:
- Dog Bacteria Could Possibly Reduce the Risk of Obesity in Owners
- Raw Food Diets: High Risk and Little Reward
This intestinal microbiota influences the health of its host by providing nutritional substrates, modulating the immune system, and supporting the body's defense against intestinal pathogens.2 By contrast, the term “microbiome” refers to the total number of microorganisms and their genetic material.
Disruptions of the intestinal microbiota can result in GI distress. According to Dr. Marks, who is a professor of medicine at the University of California, Davis, Veterinary Medical School, antibiotics are a significant destroyer of normal GI flora and function. Antibiotic use is linked to increased risk for Clostridium difficile infection, type 1 diabetes in children from repeated dosing between 1 and 2 years of age,3 and obesity, infections, asthma, and allergies in humans.
Manipulation of the Intestinal Microbiome
Therapeutic manipulation of the intestinal microbiome is a newer area of research. Efforts to maintain healthy flora or to re-balance gut microbes focus on antibiotic use, dietary manipulation, helminth therapy, fecal microbiota transplantation (FMT), and prebiotic, probiotic, or symbiotic use.
Probiotics
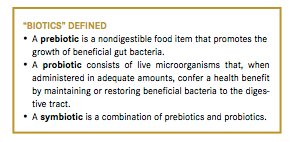
All three “biotics” are oral products. The traditional definition of a probiotic is accepted by the World Health Organization (WHO) but not the Food and Drug Administration (FDA) (see “Biotics” Defined). The FDA’s position is that the commercial development of probiotics has outpaced scientific data proving their benefit. Therefore, no approved substantiated health claims exist for probiotics in the United States.
Although the popularity of probiotics has surged in recent years, the idea that living organisms in food can be salutatory is not a new concept. During the Roman Empire, Plinius, a naturalist, advocated for fermented milk products for the treatment of gastroenteritis.4 And, more than 100 years ago, Russian zoologist Élie Metchnikoff theorized that manipulation of the intestinal microbiome with host-friendly bacteria found in yogurt could enhance health and delay senility. He also predicted the existence of bacterial translocation and anticipated theories linking chronic inflammation with the pathogenesis of atherosclerosis and other disorders of the elderly.5
Over the past 2 decades, there has been growing interest in both basic and clinical science in probiotics. This interest has led to more than 6000 publications in the biomedical literature, more than 60% of which have been published in the past 5 years, some in the top-ranking scientific journals.6 Health benefits can be gained from probiotic strains of the following genera: Lactobacillus, Bifidobacterium, Saccharomyces, Enterococcus, Streptococcus, Pediococcus, Leuconostoc, Bacillus, and Escherichia coli.
Some human probiotics such as VSL#3 and Visbiome contain 8 bacterial strains. Visbiome is intended for the dietary management of human dysbiosis associated with irritable bowel syndrome, ulcerative colitis, pouchitis, and hepatic encephalopathy. VSL#3 is designated for the dietary management of ulcerative colitis, irritable bowel syndrome, and ileal pouch.
Probiotics are purported to work via 4 methods:
- Production of various antimicrobial metabolites (eg, bacteriocins)
- Competitive exclusion of enteric pathogens
- Enhancement of epithelial barrier functionality
- Modulation of mucosal immune response
There is compelling evidence for the effectiveness of probiotic use in people to treat maldigestion, lactose intolerance, acute diarrhea in children, antibiotic-induced diarrhea, and ulcerative colitis, to name a few. Less compelling but intriguing results indicate that they may help in cases of travelers’ diarrhea, limit sepsis associated with acute pancreatitis, and aid in the prevention of postoperative infections.
Fewer studies have been conducted in dogs, most of which have involved healthy specimens. Two studies involving the use of probiotics for diet sensitivity and food-responsive diarrhea have yielded positive results,7,8 while others have shown promising, if limited, results.
We know less about cats. One study with Enterococcus faecium SF68 in shelter cats showed a significant decrease in diarrhea among treated cats versus placebo subjects. A deeper understanding of the intestinal microbiome of healthy dogs and cats versus animals suffering from GI disease is necessary before we can make specific recommendations for treatment and product use.
Veterinary professionals should remember that probiotics are not regulated by the FDA. Dr. Marks told the audience about results of a review in the Canadian Journal of Veterinary Medicine that examined 23 veterinary probiotic products. He discovered that only 17 of the 23 products listed bacterial species among the ingredients. For 3 of those 17 products the contents were misspelled, and in 8 the bacterial species were misidentified. Plus, only 5 of the 23 products listed numbers of organisms.9 While inadequate labeling does not necessarily mean poor quality, the lack of consistency is confusing at best. The study authors suggest that when selecting a probiotic, veterinary practitioners should be sure the label lists the organisms included, at least to the species level; states the number of viable organisms; and guarantees a certain number of live organisms at the time of expiration. Dr. Marks advised the audience to rely on products that report research. The most extensively researched probiotic product is Fortiflora, by Purina.
Fecal Microbiota Transplantation
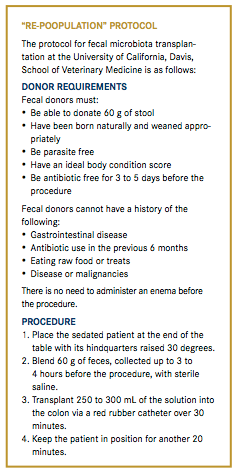
FMT, sometimes affectionately referred to as “re-poopulation,” is the transfer of fecal material from a healthy individual (donor) into the colon of a sick patient with the intent of improving health. Successfully used to treat recurrent C. difficile infection in people, veterinarians are exploring ways that FMT can help animals.
Fecal inoculation is not new. Young elephants, pandas, koalas, and hippos routinely eat maternal feces. Rabbits, hamsters, guinea pigs, and chinchillas are regularly coprophagic. Even gorillas and chimpanzees are known to eat their feces. According to Dr. Marks, there are neither guidelines nor data on the indications for FMT in dogs, but anecdotally it appears to help in the treatment of some intractable cases of diarrhea (see “Re-Poopulation” Protocol).
Future Directions
With more studies, we hope to discover the best ways to manipulate the intestinal microbiome for optimal dog and cat health. Many questions remain: Are single-strain probiotics as active as multistrain probiotics? Is there an ideal number of organisms in preparation? What is the optimum dose of bacteria for dogs and cats? Do we treat a Yorkie with the same dose as a husky? Are probiotics most helpful as a preventive measure or as treatment? Does FMT therapy offer hope for chronic diarrhea cases?
Dr. Beth Thompson is a small animal veterinarian, animal health executive, editor, and writer. She has held numerous positions with oversight responsibilities for editorial and business direction, including for Veterinary Learning Systems (publisher of Veterinary Technician and Compendium), Vetstreet.com, HealthyPet, and NAVC.
References:
- Savage DC. Microbial ecology of the gastrointestinal tract. Annu Rev Microbiol. 1977;31:107-133.
- Hooper LV, Wong MH, Thelin A, et al. Molecular analysis of commensal host-microbial relationships in the intestine. Science. 2001;291:881-884.
- Livanos AE, Greiner TU, Vangay P, et al. Antibiotic-mediated gut microbiome perturbation accelerates development of type 1 diabetes in mice. Nat Microbiol. 2016;1:16140. doi:10.1038/nmicrobiol.2016.140
- Ho N, Prasad V. Probiotics, prebiotics, synbiotics and naturally fermented foods: why more may be more. Ann Gastroenterol. 2013;26(3):277-278.
- Mackowiak, P. Recycling Metchnikoff: Probiotics, the intestinal microbiome and the quest for long life. Front Public Health 2013;1:52.
- Rijkers GT, de Vos WM, Brummer RJ, et al. Health benefits and health claims of probiotics: Bridging science and marketing. Br J Nutr. 2011;106(9):1291-1296. doi:10.1017/S000711451100287X
- Sauter SN, Benyacoub J, Allenspach K, et al. Effects of probiotic bacteria with food responsive diarrhoea treated with an elimination diet. Anim Nutr. 2006;90:269.
- Pascher M, Hellweg P, Khol-Parisini A, Zentek J. Effects of a probiotic Lactobacillus acidophilus strain on feed tolerance in dogs with non-specific dietary sensitivity. Arch Anim Nutr. 2008;62:107-116.
- Weese JS. Evaluation of deficiencies in labeling of commercial probiotics. Can Vet J. 2003;44(12):982-983.

Episode 67: Choosing trusted supplements
October 20th 2021In this episode of The Vet Blast Podcast, Dr Adam Christman chats with Dr Janice Huntingford about the latest insights into selecting the best supplements for your patients, including the importance of recommending and utilizing products that have a substantial amount of science and research behind them. (Sponsored by Vetoquinol)
Listen