
Use these links to access practice guidelines developed by veterinary organizations.
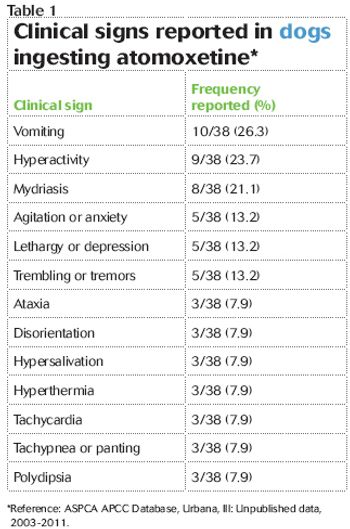
At fairly low dosages, atomoxetine-a drug in people to treat ADHD-can be toxic in dogs and cats.

Try dispensing products in biodegradable waste disposal bags.
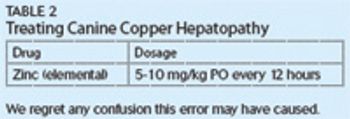
The dosage for zinc (elemental) was listed incorrectly in Table 2 of this article.

Dr. Miller knows many of you will scoff at the surprising confirmation that Bigfoot exists.

Training exercise provides needed vaccinations for local livestock.


This study looked at whether such a screening is worth it and what it means if the results are negative.

Client handout: Parasites at a glance
Online resources for veterinary students.

Insurance companies host events in Las Vegas to recognize veterinary honorees.

Facility adds more veterinary research space in addition to NBAF now under construction.
Stress, fatigue, and irritability sometimes cause veterinarians to lost their tempers.

Check out these animal mascots for the Sweet Sixteen teams in the 2013 NCAA tournament

Skunk spray is toxic? Be prepared-your next patient may be skunked!

Create a list for those downtimes at your practice.

This reader idea will help you to find the right size catheter right away.

Despite being apparently healthy, middle-aged and older cats can often have abnormalities that would benefit from intervention and monitoring.

An attempt to put some numbers to the predatory nature of domestic free-ranging cats.

Learn when decontamination with activated charcoal will benefit your patients and how to best administer it.

Save a little money and a lot of time with this reader tip.
Dr. Robert Miller's take on the popular reality show The Incredible Dr. Pol.

The dogs and their handlers arrived the day after the tragedy and remain at Sandy Hook still.

Golden retrievers receive extensive training and veterinary care.

Clinical interest in this glucocorticoid stems from its immune-modulating effects directly at the level of the intestinal tract with few of the systemic effects typically associated with corticosteroids.

Download this list of 20 critical parameters to evaluate in critically ill patients every day.

This procedure is not only useful for breeding purposes but can also help you detect problems in a dog's prostate gland.

Eager to show their expertise, veterinary clients help diagnose a poisoned dog.

Reference list for "Rethinking your approach to perioperative fluid therapy"