“Y” is for your dental operatory—you’ve got to take care of it, and it will take care of your patients
An expert in veterinary dentistry outlines the importance of caring for your machines and accessories to facilitate safe, effective dental procedures.
The dental operatory is an area with special equipment and facilities to perform dental diagnostics and treatment. Care and maintenance of the equipment and materials in this room are essential for successful dental procedures and safe delivery of anesthesia. This article focuses on getting consistent, accurate results from your anesthesia monitors and machines through careful inspection and maintenance. The second half of the “Y” is for… series will cover preventive care for your dental delivery system, handpieces, dental surgical instruments, and intraoral imaging sensor(s).
Anesthesia safety
Anesthesia safety is probably the top concern on clients’ minds regarding dentistry. Your clients may think that because they are not anesthetized when they go to the dentist, why should their dog or cat need general anesthesia for a case of halitosis? The answer is “to thoroughly examine and treat (any) subgingival disease, which is not possible without anesthesia.” Safely performed, professional oral prevention, assessment, and treatment rely on choosing the right patient, the right anesthetic protocol, and proper monitoring during and after anesthesia.
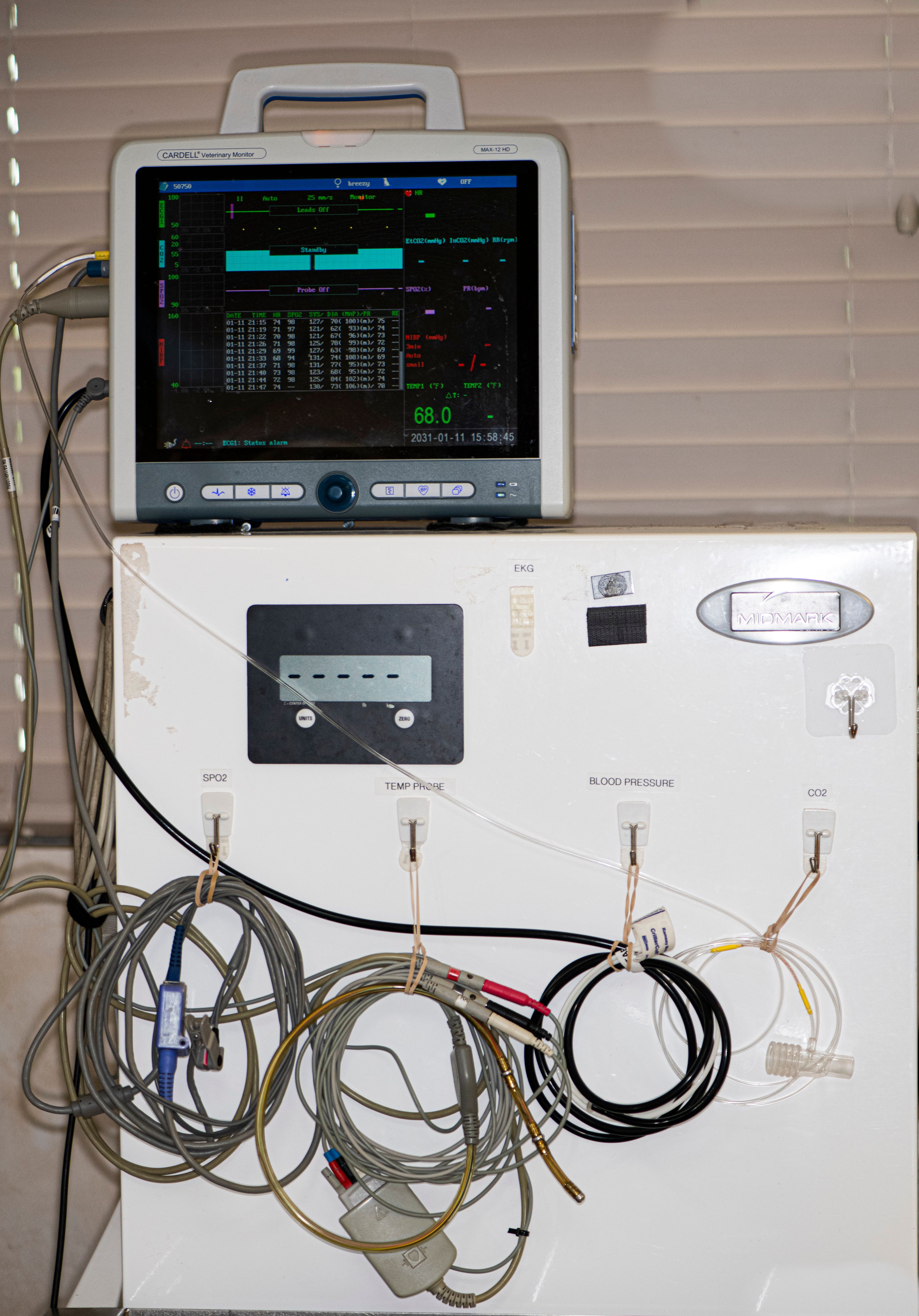
The monitor
Purchasing the best anesthetic units and monitoring systems is not enough to ensure consistently positive experiences. Out of the box, monitors generally work flawlessly with large and bright electrocardiogram (ECG) tracings, loud and regular audible beeps, the pulse oximeter, and consistent measurements of blood pressure and end tidal CO2. Sometimes, months after the purchase, you look up at the screen and can barely read the ECG, the CO2 end tidal volume alarm is constantly being triggered, and there is no evidence of blood pressure measurements. What is wrong with these units? Generally, the problem with the units is not the manufacturer. It is the way we maintain the peripheral attachments, and how we train our surgical assistants to perform anesthetic monitoring.
The monitor’s accessories are considered consumable items and, based on their direct contact with patients, are subject to wear and tear. They need to be replaced from time to time. This is a harsh reality for many who are used to paying for the highest quality equipment and expecting everything to work seamlessly without much additional effort or expense. How the accessories are cared for directly affects the frequency and expense of replacement.
For example, the rate at which we (at All Pets Dental) were replacing pulse oximeter sensors seemed exceedingly high. At $250 each, we needed to do better, and made sure that every staff member was trained and held responsible for their proper care.
Figure 1a. SpO2 tip-clip sensor. Not using the tension clip will cause the sensor to fray where the lead meets the sensor. Using a sensor that is frayed can cause injury to the patient and possible burns to the area at which the sensor is applied. It also can cause inaccurate readings and dropped measurements. This sensor is dirty with dried blood; daily cleaning is necessary.
Figure 1a.

What we have learned:
- We have learned the hard way to buy monitors manufactured in the United States. For us, buying cheaper monitors from overseas resulted in poor unit life span, inaccurate results, and impossible service. Tip: Buy from US manufacturers that ensure 3- to 5-day repair turnaround.
- Much of the damage to handheld units came after the instruments were accidentally dropped on the floor. Consider options for mounting and protection and opt for table mounts and rubber covers. The cost of 1 repair could easily cover that expense.
Figure 1b. Stationary table mount.
Figure 1b.

- For us, the best approach to monitor responsibility and care was to designate the role of anesthesia unit and monitor equipment specialist to one of our technician assistants. In addition to meeting with and training all those who handle the monitors, the monitor equipment specialist (on a nonsurgical day) completes a weekly checklist to ensure that each unit is fully functioning. If a unit is not fully functioning, the specialist would bring this to the attention of the practice manager after calling the vendor for advice.
Figure 2. Training staff on the operation and care of each monitor.
Figure 2.

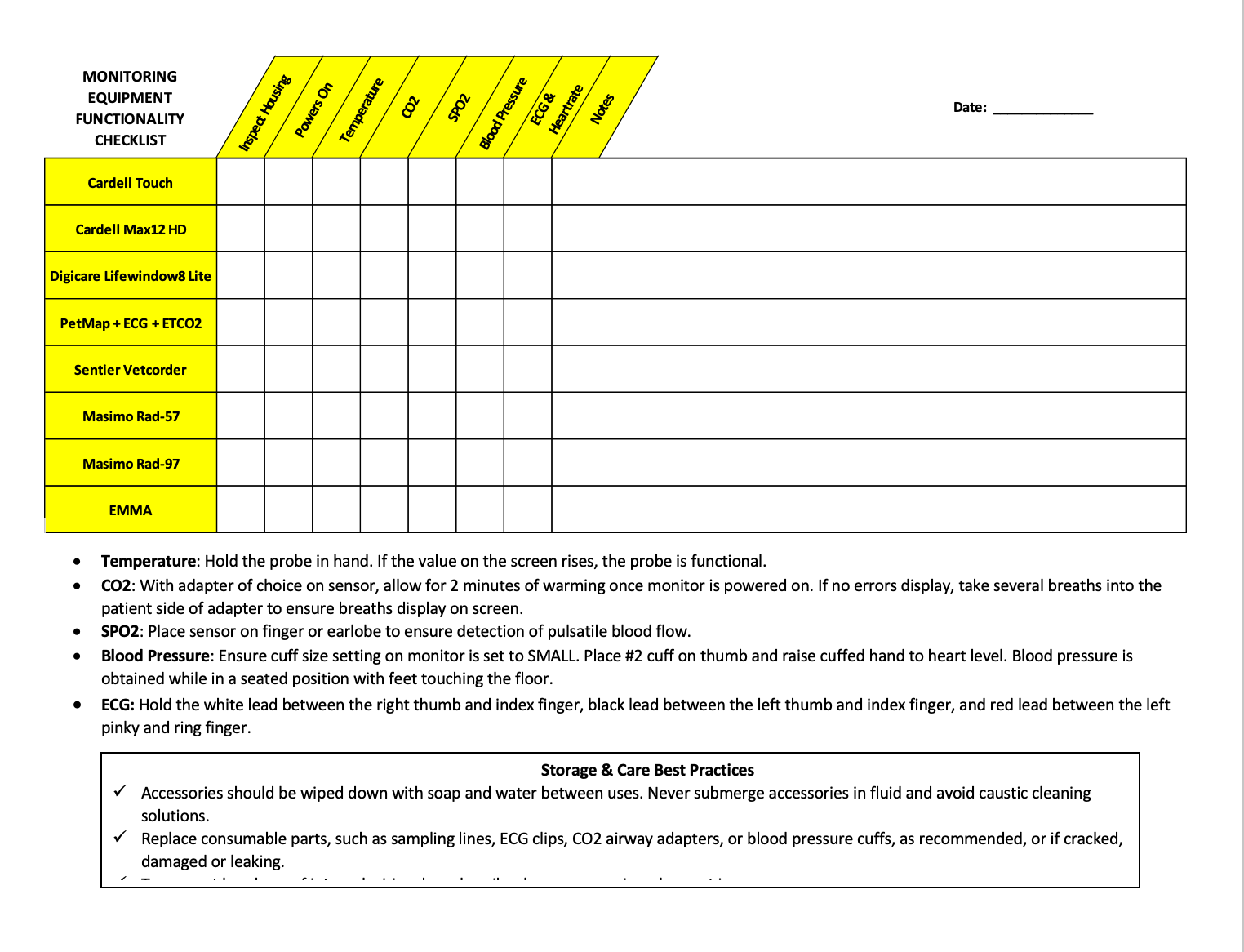
Figure 3. Weekly monitor checklist.
Figure 3.
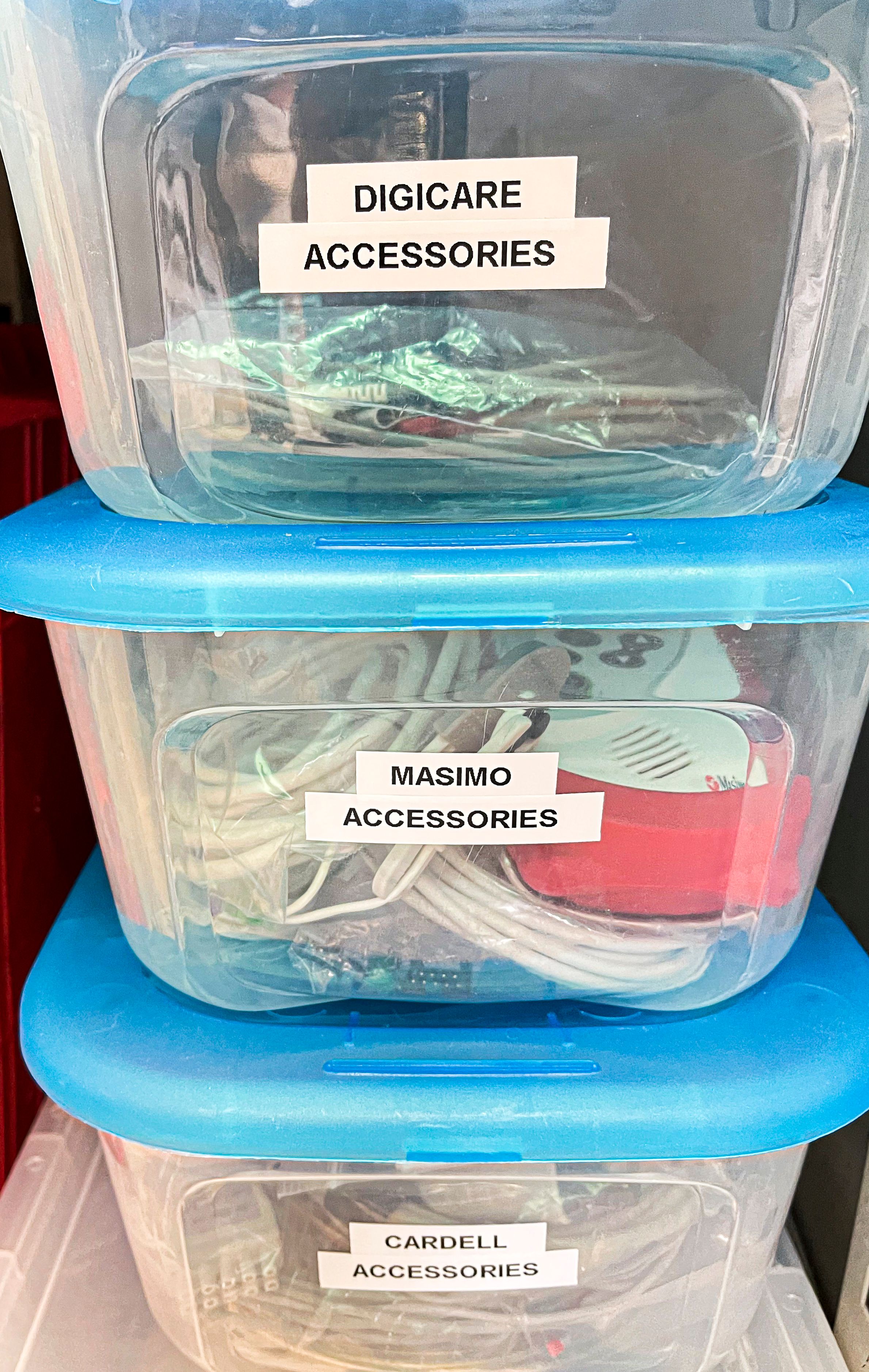
- Because most practices have monitors from multiple suppliers, consider keeping additional peripherals, blood pressure cuffs, and repair items associated with a particular monitor together in a large transparent plastic container. Care should be taken to avoid any interchange of the accessories from one monitor to another unless they are 100% compatible. This is especially true for power supply/charging units. Even if the connector is compatible, severe damage can occur with a power overload.
Figure 4. Transparent plastic containers to keep peripherals for each monitor separate.
Figure 4.
Care and maintenance of peripheral accessories
Blood pressure cuffs
When the Velcro on the blood pressure cuff is worn out, it is time for a replacement. Taping the cuff will yield inaccurate readings. In addition, pay close attention to how the blood pressure cuffs are stored after use. They should be disconnected from the unit and stored flat. Storing them on the unit often creates abnormal stress on plastic surfaces.
Tips:
- Keep blood pressure cuffs clean by wiping with alcohol after each use.
- Replace cuffs if damaged, worn, or unable to be thoroughly cleaned or disinfected.
- Replace cuffs if the 2 sides of Velcro do not properly adhere to each other—never tape a cuff.
- Be sure to follow manufacturer guidelines for cuff size and placement.
- Always use the cuffs provided by the manufacturer.
- Never place a cuff on the same limb as the Sp02 sensor orcatheter.
Figure 5. Noninvasive blood pressure cuff with hair on the Velcro, making it unable to hold continuous contact. This cuff is dirty and, even after being cleaned, remains discolored. In addition, the hose to this cuff is loose, causing it to have a possible air leak and deliver inaccurate measurements.
Figure 5.

CO2 sampling lines
A good rule of thumb: as soon as an occlusion alarm is triggered, replace the sampling line. If visible moisture is evident beyond the neoprene filter, hang the line to dry. Failure to do so would increase the chances that the moisture will reach the internal module and burn out the circuitry.
Tips:
- Monitors equipped with side stream CO2 sample lines should be disconnected and the mouthpiece hung downward to dry.
- Never force air through the line to expedite drying, because it can destroy the filter.
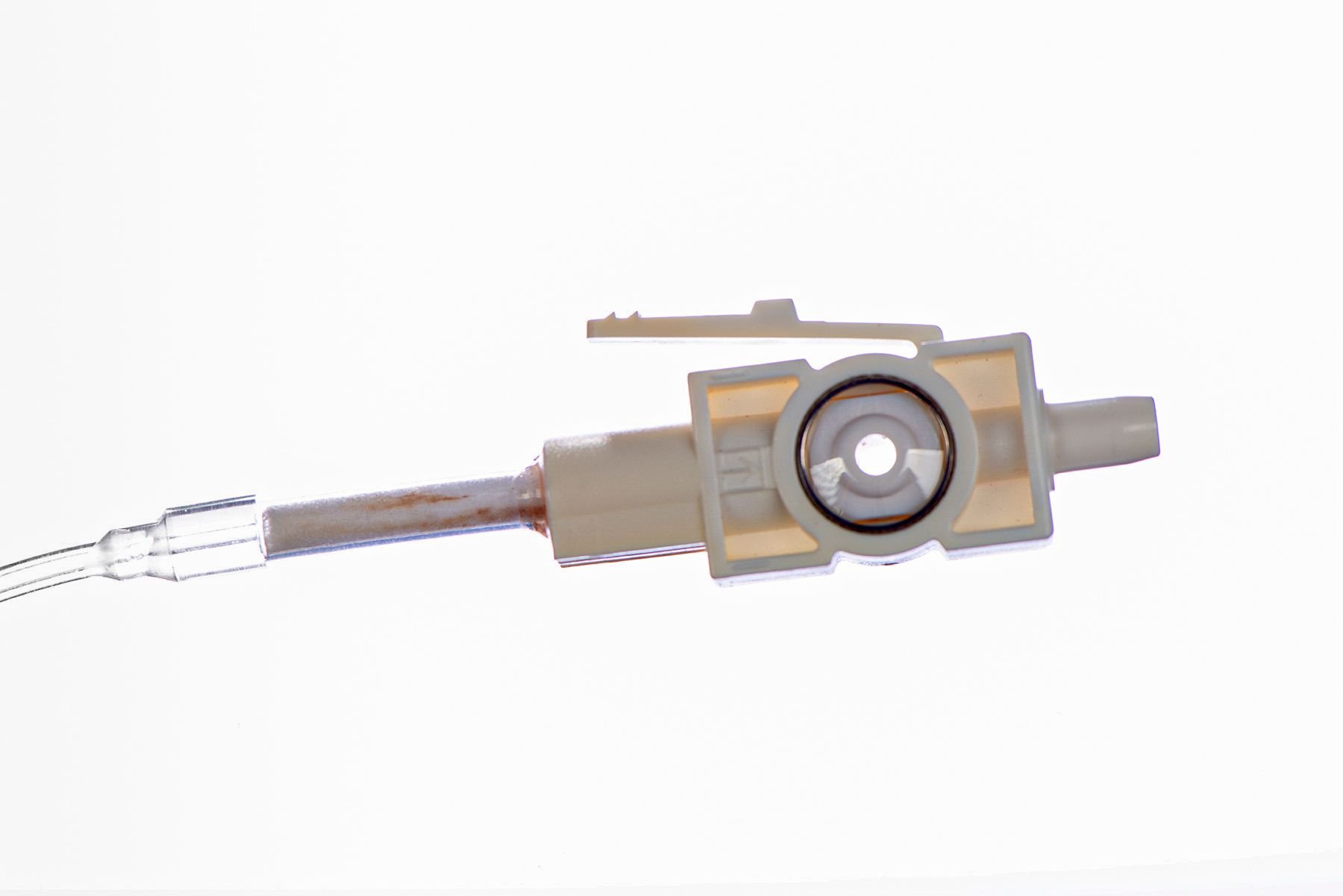
Figure 6a. The sample line was damaged and then taped. This causes inaccurate measurements. The filter is yellow and dirty because of excessive moisture and use, which will cause inaccurate readings and occlusion in the sample line.
Figure 6a.
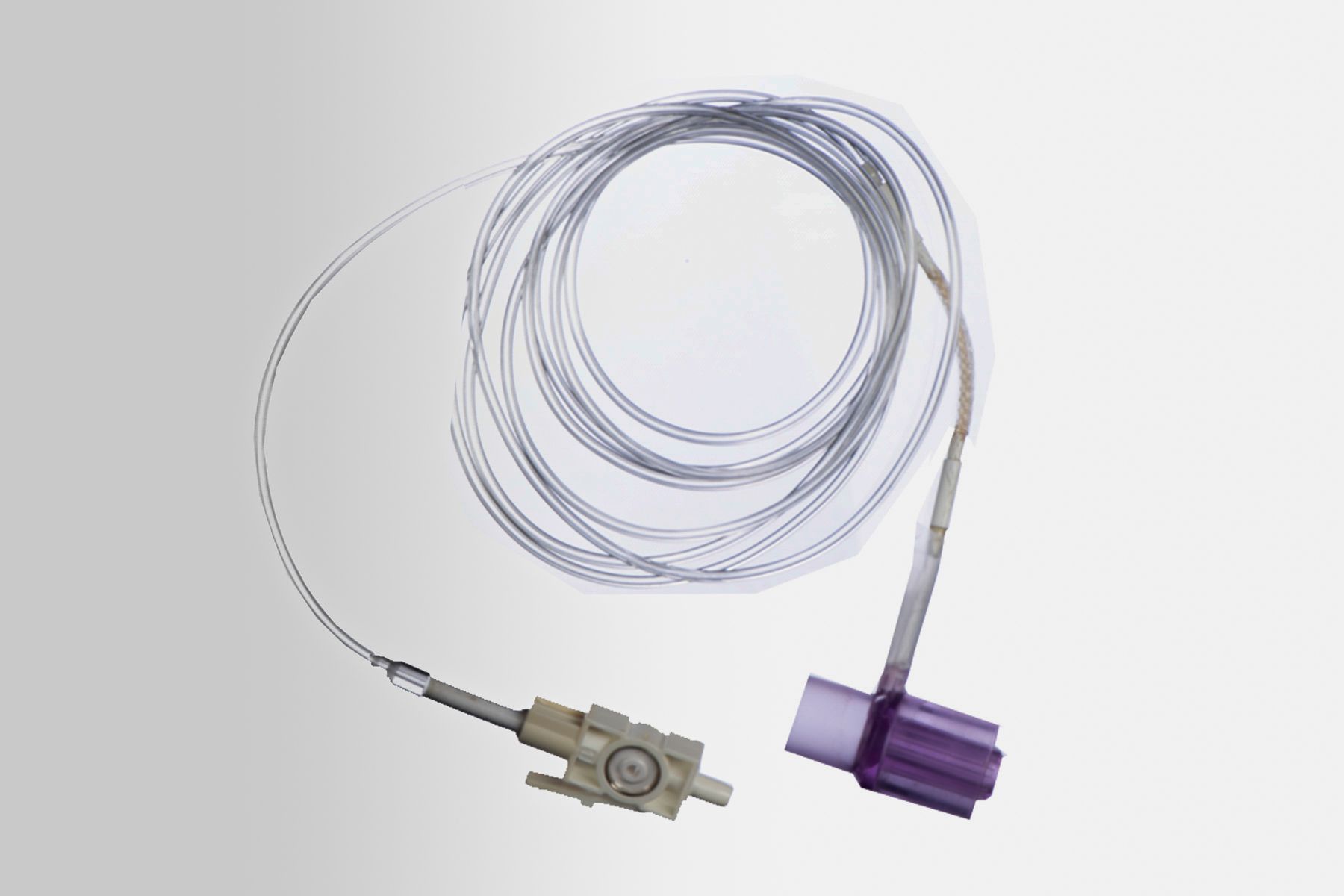
Figure 6b. Close-up of filter damage.
Figure 6b.
ECG leads and clips
Green or black buildup on copper clips can be part of normal oxidation that should be regularly cleaned, or it can mean your staff is mistakenly using ultrasound gel (acoustic gel) rather than electrode paste (conductive) to maintain good contact. Ultrasound gel will not only block the electrical signal but will also quickly degrade the clips.
Tips:
- Clean clips daily by gently wiping with alcohol or by using an instrument brush.
- Never wind tightly to store, and never use ultrasound gel instead of electrode gel.
Figure 7. Electrocardiogram (ECG) clip damage secondary to excessive use without cleaning between patients and using alcohol instead of ECG gel, which causes faster corrosion of the metal. This clip is rusted and so is the spring, which can cause damage to the patient’s skin as well as inaccurate readings.
Figure 7.

Pulse oximeter sensor
When the infrared light on the pulse oximeter sensor is intermittent, it is because the thin internal wires are usually frayed or are being pulled apart at the junction, a precursor to complete sensor failure. Always have a spare pulse oximeter sensor. Having a working spare will also allow you to troubleshoot the parameter to eliminate the possibility that the problem resides in the monitor itself.
Tips:
- Wipe the sensor clean with alcohol daily; never use other cleaners that may damage plastic. Never wind tightly or pull clips off when changing them.
- Be sure to unclip before moving the patient.
- Use the tension clip on the cable to avoid damage to the patient’s skin and avoid fraying.
- Avoid using the lingual sensor in the mouth during dental procedures; tail sensors are ideal for use during dental procedures.
- To avoid pressure damage, the sensor should be repositioned every 20 minutes.
Figure 8. Management of peripheral wires after use; a) rolling stand with coiled wire storage (Digicare); b) close-up showing hooks; c) wires attached with wraps on lift table.
Figure 8a.

Figure 8b.

Figure 8c.
Anesthesia machine
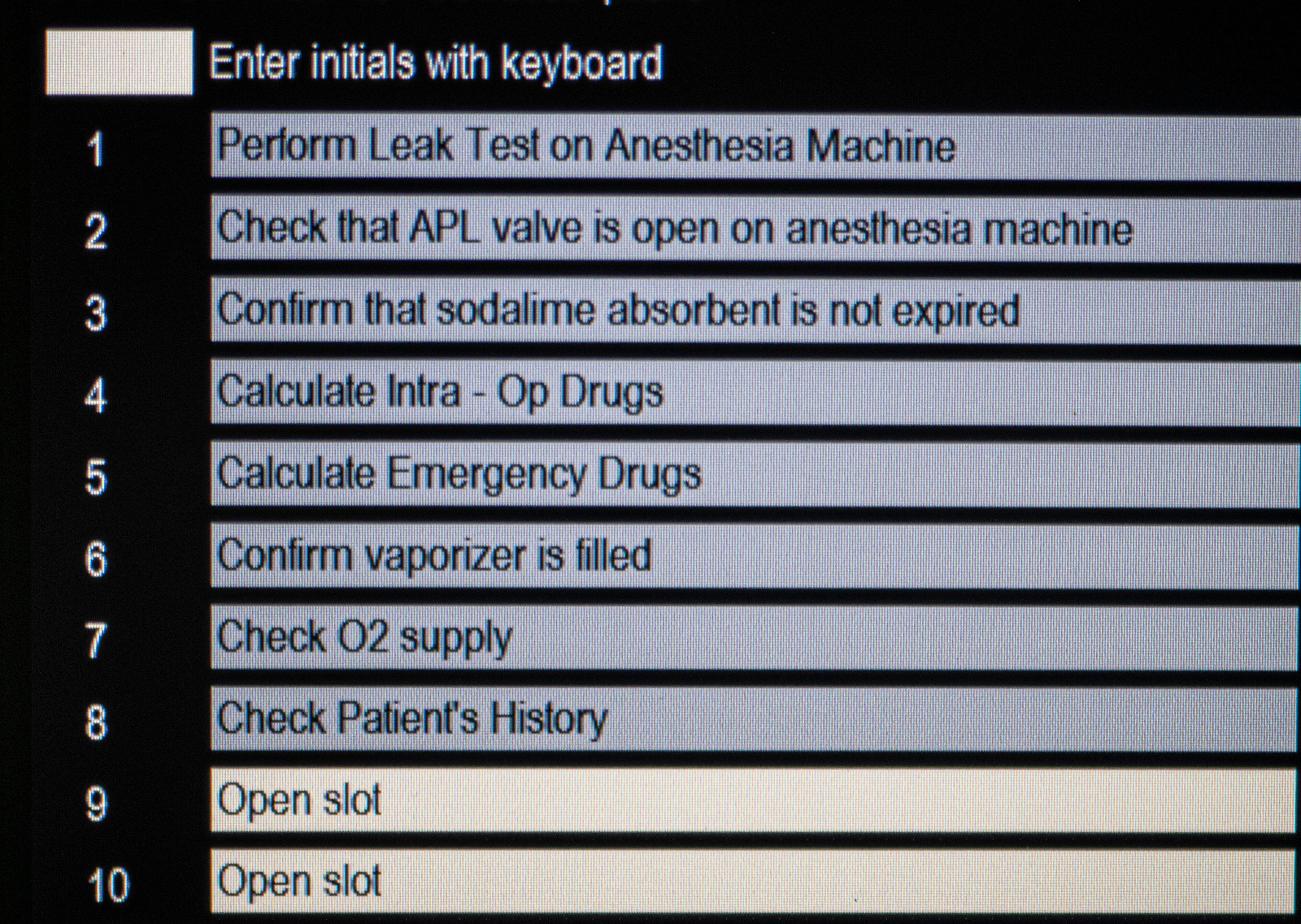
Similar to a pilot examining a plane and completing a checklist, consider adding an anesthesia unit checkup before the patient is anesthetized. A recently released monitor unit would have the checklist incorporated and allows a manual checkoff before monitoring commences.
Figure 9. Check off list before anesthesia is commenced.
Figure 9.
The leak test
A leak test should be performed before every procedure. By verifying that there are no leaks in the machine, you allow the technician/doctor to administer the correct flow rate of oxygen and percentage of inhalant drug to the patient. Leaks are not only wasteful but can compromise the safety of the patient and staff.
Tips:
- Perform a leak test between each procedure.
- Replace the maintenance kit at least annually, including the black rubber tubing, domes, gaskets, flutter, and discs.
- The rubber parts should be cleaned daily with mild soap and water.
Breathing bag and breathing circuit
The breathing bag and breathing circuit should be washed and hung to dry after each procedure. If a bag/circuit is used for successive procedures without being cleaned, infections can be passed between patients.
Tips:
- If a tear is evident in a bag or breathing circuit, that particular bag/circuit should be replaced.
- Taping the circuit or bag may continue to allow a leak in the system and waste oxygen and the inhalant drug.
CO2 absorber
CO2 absorbent granules are designed to “scrub” the expired gases of CO2, and the reaction causes the granular absorbent material to change color (bluish gray or purple) as a visual guide. The absorbent material can be depleted after a matter of hours, and will return almost to its original color overnight, a phenomenon known as regeneration. Depleted granules are hard to the touch and not easily crushed when pressed between the fingers, as compared to fresh absorbent. Channeling of gases may occur, leaving the visible granules against the sides of the canister fresh, while the gases pass through the expired granules toward the center, sending increased levels of CO2 back to the patient.
Tip:
- Keep a log sheet next to the machine and replace the absorbent every 6 to 8 hours of use.
Vaporizer
To ensure the accuracy of anesthesia delivery, the vaporizer should be professionally serviced and certified on an annual basis by the manufacturer. Some companies have an exchange program through which they send you a reconditioned vaporizer in exchange for the one in current use. Failure to make this exchange could result in patients being too “light” (and waking up in midprocedure) or too “deep,” which could compromise vital organs.
Handling the costs of quality maintenance
On all our invoices, there is a line item for hourly anesthesia monitoring. This allows our practice to update and maintain our anesthesia and monitoring equipment and accessories. Paying close attention to the care of your monitors makes sense for the patient, staff, and practice.
The author thanks Andrew Schultz Jr (Midmark), Amanda Goetz and Eduardo Miranda (Digicare), and Jerry Maass (petMAP) for assisting in the preparation of and providing images for this article (Digicare and Midmark).
Jan Bellows, DVM, DAVDC, DABVP, FAVD, owns All Pets Dental in Weston, Florida. He is a diplomate of the American Veterinary Dental College and the American Board of Veterinary Practitioners. He can be reached at (954) 349-5800; email: dentalvet@aol.com.

