Clinical case study: Radiation therapy for facial mast cell tumor in a beagle
From the clinical examination to procedure and treatment methods to the outcome, discover this beagle’s experience undergoing radiation therapy for an MCT.
A 10-year-old castrated male beagle was evaluated by the oncology service at the Animal Referral Hospital in Sydney, Australia, in June 2020 for a large subcutaneous mass on the left rostral muzzle. The mass was first detected by the dog’s owner in May 2020. Subsequently, they noticed a waxing and waning of the swelling before the mass was evaluated by their family veterinarian.
Figure 1: The patient, pretreatment, with the area of the mass circled in red.

In-house cytology had been performed by the veterinarian, and the cells were consistent with a mast cell tumor (MCT). Owing to its size, location, and extension into the oral mucosa, the mass was not considered to be surgically resectable, and the patient was referred to the Animal Referral Hospital for further assessment and discussion of treatment options.
Clinical Examination
On presentation, the patient was bright, alert, responsive, and hydrated. The mass measured approximately 5 cm in diameter and was subcutaneous, with a significant component extending into the buccal and labial oral mucosa of the left rostral maxilla, as manifested by erythema and swelling. The ipsilateral mandibular lymph node was mildly asymmetrically enlarged. Other aspects of the clinical examination were unremarkable.
Procedures
A fine-needle aspirate of the left mandibular lymph node was performed, and the results of cytologic evaluation were consistent with metastatic MCT. A complete blood count and blood chemistry panel were performed, and all results were within normal limits. An abdominal ultrasound exam was then performed to complete staging; it was all clear. The patient was considered a good candidate for radiation treatment of the MCT, and the patient then underwent a CT scan for radiation treatment planning.
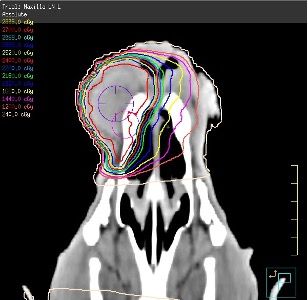
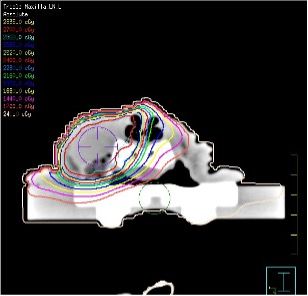
Figure 2a & b: CT scans showing the mass.
Treatment
A course of stereotactic radiation therapy was initiated to treat both the local MCT and the left mandibular node and was completed 2 days later. The mass received 3 × 9 Gy for a total of 27 Gy, and the mandibular node received 3 × 8 Gy for a total of 24 Gy.
When the treatment was completed, the patient was started on prednisolone 0.5 mg/kg once daily and continued on fexofenadine (Telfast) 180 mg twice a day. The prednisolone was weaned down over the next 3 weeks, but the patient remained on antihistamines throughout the course of treatment.
Adjuvant chemotherapy with single-agent vinblastine was started 2½ weeks later and completed after 11 weeks. The patient received the first 4 doses (2 mg/m2) intravenously on a weekly basis, and the final 4 doses were administered every other week at the same dose.
Restaging with abdominal ultrasound performed halfway through the chemotherapy regimen showed that the patient remained in clinical remission for local disease with no evidence of distant metastasis.
Outcome
The patient tolerated the radiation treatments very well and showed no obvious acute effects at the time of completion of therapy. However, some effects did start to manifest in the subsequent 2 to 3 weeks with alopecia in the treated field and mild to moderate oral mucositis with mild sloughing of the oral mucosa.
Figure 3: The patient 2 weeks after radiation therapy.

The mass went into complete clinical remission within 10 days following completion of the course of radiation therapy. The oral mucositis resolved within the next 3 to 4 weeks. A focal, 5 mm mucosal erosion persisted in the left upper lip for the next 3 months, after which it was completely healed.
Figure 4: The patient 3 weeks after radiation therapy.

The alopecia within the field became more extensive and significant dermal hyperpigmentation in the left rostral muzzle also became evident and persists.
The patient is in clinical remission and continues to do well 11 months after starting radiation therapy.
Figure 5: The patient approximately 9 months after initial assessment at the Animal Referral Hospital.

Discussion
MCTs are a common type of skin cancer in dogs. Many MCTs are considered locally invasive and can be difficult to completely remove surgically due to the extent of local disease and challenging anatomic locations involved.
As this patient’s tumor was subcutaneous as opposed to dermal in origin, traditional grading of the mass with biopsy would have been of limited prognostic value. However, reports have linked MCTs involving the oral mucosa with a more aggressive biologic behavior. Indeed, this patient was shown to have metastasis to the ipsilateral mandibular lymph node.
However, as the disease had not progressed to involve internal organs, a combined chemoradiation treatment regimen was considered the best option. Mast cells are very sensitive to ionizing radiation and generally shrink rapidly and substantially with this treatment alone.
Although several new treatments for MCTs are available, such as tigilanol tiglate (Stelfonta), the extensive tissue trauma and uncertainty of effective tumor margin coverage associated with intralesional injections made this a less desirable option for this patient.
Furthermore, given the lymph node involvement, it was considered prudent to treat with a systemic chemotherapy regimen as well. To date, the outcome for this patient has been as expected, but ongoing monitoring will be done to assess for any signs of relapse, as early detection can lead to the best outcomes.
David Lurie, BVSc; Diplomate, ACVIM (Oncology); Diplomate, ACVR (Radiation Oncology), works at the Animal Referral Hospital in Sydney and is 1 of only 2 veterinarians in Australia who hold specialist qualifications in both veterinary medical and radiation oncology. He was also the first veterinarian in Australia to hold this dual specialist certification.
Clinical case sub-edited by Phil Tucak, BSc, BVMS, an Australian veterinarian, communications manager, and veterinary journalist. As the Wildlife Outreach Vet, he works to share the conversation about conservation. Phil is DVM360’s freelance Australian correspondent.
