Stopping the otitis snowball: identifying the infection and cause
The ins and outs of otitis, plus the benefits of hand-held otoscopy.
Five or more dogs on your schedule for the day? Chances are, at least 1 of them has otitis.1 To set them up for short-term recovery and long-term management, we’ll walk you through identifying underlying factors, examining the patient, taking appropriate samples, and using imaging or referrals when necessary. Keep an ear out for the upcoming otitis externa consensus guidelines from the World Association of Veterinary Dermatology as veterinary medicine continues to evolve.
Would a hair pluck help?
Hair follicles are a normal component of the external ear canal. They’re often simple follicles, but there can be excessive compound hair follicles in some dog breeds.3,4 Although the presence of excessive hair can be a predisposing factor for otitis, plucking can cause inflammation in the ear canal, making the ear even more prone to bacterial or yeast colonization and proliferation.1,5 The presence of hair in the ears alone would not cause an infection, as evidenced by the many hairy-eared asymptomatic humans, so routine hair plucking is not recommended.
Examining the otitis patient
Getting the whole picture
Relevant history questions6 :
- Is the infection in one ear or both?
- When was the ear disease first noticed or diagnosed? What were the symptoms? (eg, headshaking, scratching, neurologic signs, lethargy, pain when opening the mouth, etc)
- Is this the first occurrence of ear disease? If not, when were the previous episodes? Is there a seasonal pattern?
- Have medications been used previously? If so, what was the clinical response? Any adverse effects?
- Has the pet received a previous diagnosis or been treated for an underlying disease that would lead to ear infections? (eg, allergies, hormonal disease, etc)
- Are there any other skin lesions or pruritus?
- Is the pet otherwise systemically well?

Relevant physical exam findings5,6
- Check common concurrently infected areas: face/body folds, ventral neck, axillae, ventrum, perineal region, nailbeds, paws.
- Check ear(s) for pruritus, erythema, pain, head shaking, malodor, discharge, excoriations, pinnal changes, stenosis, masses, aural hematoma, ceruminous cystomatosis.
- Document palpating soft normal versus thickened firm/hard external ear canals, particularly in a multidoctor practice, to ensure continuity of care. Thickening can signify that the ear is approaching end-stage disease.
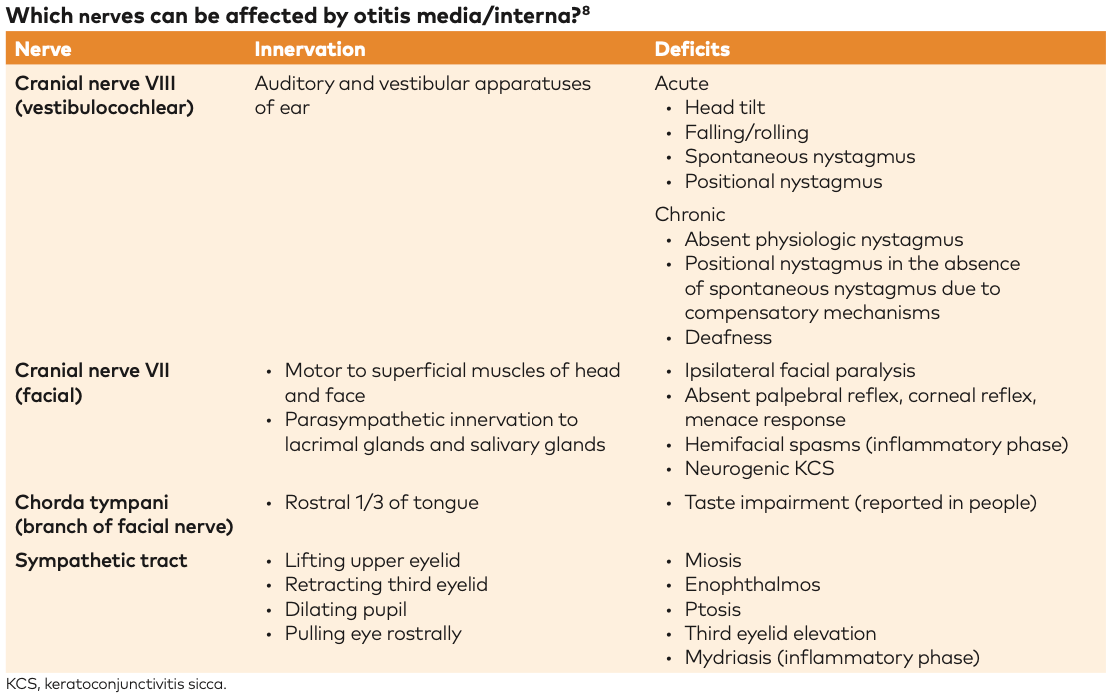
- Check for signs of nerve involvement: cranial nerve VII/VIII deficits (see chart below), Horner syndrome, keratoconjunctivitis sicca, dull/lethargic (central).
Anatomy encountered during otoscopic examination
The external ear canal extends from the outer opening to the tympanic membrane. The intertragic incisure serves as a landmark from which to start an otoscopic exam.3,4 A helpful tip during otoscopy is to retract the pinna dorsally and laterally to straighten the canal. This allows the scope to pass unimpeded by the dorsal fold, the prominent dorsal ridge of cartilage at the junction of the vertical and horizontal canals.4,5
When visualizing the tympanic membrane:
- the pars flaccida, located dorsal to the pars tensa is small, opaque, pink, and vascular1
- the pars tensa, located ventral to the pars flaccida is small, dark, translucent portion of the tympanic membrane, and3,5
- the stria mallearis, the outline of the manubrium of the malleus, visible through the pars tensa. It is concave rostrally in dogs and straight vertically in cats.4
How is an otoscopic exam completed on a nonadherent patient?
Proper restraint is key to a thorough otoscopic examination, particularly for a patient in pain.3 Restraint is best achieved by covering the dorsal muzzle with the palm of the hand, with the thumb and fingers directed downwards on opposite sides of the muzzle. Angling the head downward and restraining from above prevents a strong, quick elevation of the muzzle during otoscopy, which is a common reaction.5
As with any diagnostic test, it’s important to consider what the clinician and client would do with the obtained information; for many ear cases, short-term management may not change much. For this reason, the authors typically do not sedate fractious patients solely for an otoscopic exam, unless there is also a plan for treatment while under sedation (eg, cytology, blood work, leave-in ear meds, etc.). For painful infected ears, it may be best to treat first, then recheck with pre-visit pharmaceuticals. See below for a discussion of general anesthesia for ear flushes.
How is an otoscopic exam completed when the ear canal is full of debris or too inflamed?
Debris in the ear canal, which limits visualization, may be removed by ear flushing.3 However, this may require anesthesia if the patient is in excessive pain or if there is a concern of possible tympanic membrane rupture.3 If excessive swelling or hyperplasia obstructs the ear canal evaluation, then topical or systemic glucocorticoids are indicated. Potent glucocorticoid treatment, whether topical (eg, fluocinolone, mometasone) or systemic (oral prednisone 1-2 mg/kg/d, ~4-7 d tapers), may be used for the treatment of acute inflammation.1 After initial control, there may be a de-escalation to topical steroids or systemic low-dose prednisone every 48 hours pending further management.1 In the authors’ opinions, glucocorticoids are more helpful for pain and inflammation than nonsteroidal anti-inflammatory drugs in the majority of ear cases.
Why are there ulcers in the ear canal?
Ulcers may suggest a Gram-negative bacterial infection, most commonly Pseudomonas aeruginosa. Iatrogenic trauma from overzealous cleaning or contact reactions (splash pattern on the pinna) should also be considered.3
What can cause a mass effect in the ear?
Tumors can be a common cause of chronic unilateral otitis externa.3 If the mass is obstructive and contributes to secondary issues (discomfort, infection), it is not entirely benign, even if it appears as such on a cellular level. In the authors’ real-world experience with obstructive tumors, if the client cannot financially afford a multistep process of incisional biopsy followed by additional workup, then complete excisional surgery should be discussed at the start.
Most ear canal tumors in cats are malignant (87.5%), whereas roughly 60.0% of ear tumors in dogs are malignant.7 Ceruminous gland tumors are the most common tumors of the external ear canal in both dogs and cats.3 Non-neoplastic diseases that may be encountered include ceruminous gland hyperplasia or cysts, inflammatory polyps, and nodular hyperplasia of the sebaceous glands.3
Is it the tympanum or a mass?
An engorged pars flaccida should be distinguished from a mass or polyp protruding from the tympanic membrane or originating from the external ear canal.1 The pars flaccida may become edematous or bulge, which may indicate an underlying hypersensitivity or fluid within the tympanic cavity.1 Particularly in the Cavalier King Charles spaniel, a bulging pars flaccida should raise suspicion for primary secretory otitis media, caused by the formation of a sterile mucus plug within the middle ear.8
How is the patency of the tympanum assessed? This is more of an academic rather than a routine clinical test. Besides otoscopy, patency may be evaluated with tympanometry. Tympanometry has poor sensitivity and specificity for identifying a ruptured tympanum but can be performed with readily available materials, such as a polypropylene catheter or soft red rubber catheter.1,5 If the tympanic membrane is intact, then the catheter will meet resistance. If the tympanic membrane is ruptured, then the catheter will enter the bulla ventrally.1
What are the benefits of video otoscopy compared with handheld otoscopy?
Handheld otoscopy remains an important, quick, inexpensive, and readily available tool for routine exams. However, for challenging ear cases, video otoscopy offers superior optics through greater magnification and detail, while maintaining a visual field for irrigation, and ports for instrumentation.3 These features help to increase the safety of procedures within the ear canal, such as the removal of foreign objects, debris, or parasites using grasping forceps; biopsy collection with biopsy forceps; CO2 laser surgery with specialized attachment tips; or guided myringotomy with a spinal needle.3 Because the images are projected onto a screen with the capabilities of image capture, recording, and printing, it has been suggested that video otoscopy increases client participation, which may translate into increased client compliance.1,3
When is anesthetized evaluation of the ear canal indicated?
Anesthesia is indicated for deep ear flushing.3 A cuffed endotracheal tube protects the airway from contaminated fluid traveling from the Eustachian tube into the nasopharynx through a known, unknown, or iatrogenic tympanic membrane perforation.3 Sedation is not a reasonable alternative, as it impedes the animal’s ability to protect the airway, thereby posing a significant risk factor for aspiration pneumonia.3
Indications for deep ear flushing include foreign bodies that cannot be retrieved when the patient is awake, severe acute otitis, purulent discharge or debris that obscures visualization and treatment, peripheral vestibular symptoms, Horner syndrome, and recurrent or chronic otitis.1 The goal of flushing is to remove excessive cerumen, infectious organisms, proteolytic enzymes, previous medication residue, and exudate—all of which can be irritating, mask foreign bodies or tumors, serve as a nidus for infection, or reduce the efficacy of medications.1,3 Deep ear flushing may be an indication for referral to a veterinary dermatologist with access to a video otoscope, for both short-term and long-term management.
Which anatomical areas of the ear cannot be examined with otoscopy alone?
Beyond the tympanic membrane, the middle ear consists of the epitympanic recess, which contains the auditory ossicles, the tympanic cavity proper, and the ventral air-filled tympanic bulla.1,4 The septum bulla delineates the tympanic cavity proper from the ventral cavity; this is an incomplete osseous ridge in dogs but is nearly complete in cats. This is clinically relevant for the treatment of otitis media in cats as the ventral cavity typically cannot be cleaned or sampled without the surgical approach.4 Nevertheless, results from more recent research indicate that medical management can sometimes be successful.9 The musculotubal canal is the exit point of the middle ear, opening rostrally to communicate with the nasopharynx.4
How can deafness be detected?
Infection alone can lead to deafness, but it can also be iatrogenic (eg, aminoglycosides, particularly gentamicin, loop diuretics, antiseptics, antineoplastic agents).11 Brainstem auditory evoked response testing can be used to identify conductive or sensorineural deafness, but it tends to be an academic pursuit, given the lack of treatments for deafness in veterinary patients.10
Sampling the otitis patient
Otitis externa – cytology
Cytology is a valuable tool because of its simplicity, practicality, low cost, and rapid turnaround time.12 It should be performed for every compliant patient presenting with clinical signs of otitis externa.12 Exudate characterization and odor are not reliable alternatives.1,12
How should cytology samples be collected? Samples should be collected before the introduction of any cleaning agents or therapies.12 Patients presenting with otitis externa should have both ears evaluated, even if they have unilateral disease.12 Collection from deeper within the canal is more clinically relevant but harder to obtain. The safest method of collection to maintain consistency is to aim for the junction of the horizontal and vertical ear canals by keeping the pinna relaxed and directing a cotton tip applicator ventrally through the intertragic incisure.12
How should cytology be prepared?
Ear cytology slides may be stained with either modified Wright stain or Gram stain.12 Heat-fixing has been shown to have no significant difference on cytology results.13 A modified Wright stain (eg, Diff-Quik) is clinically the most practical, as it is simple, rapid, stains the relevant cells (bacteria, yeast, leukocytes), and is easy and quick to perform in-house.12
What features are considered ‘normal’ on ear cytology?
Gross evaluation of a healthy ear will reveal a thin layer of waxy yellow to light brown cerumen, which microscopically contains normal, possibly rolled, cornified squamous epithelial cells.12 Melanin granules, if present, can be differentiated from bacterial cocci by focusing through them (ie, adjusting the fine focus of the microscope up and down); they will have a yellow to brown appearance at some depths while bacterial cocci are uniformly basophilic.12 Confounding debris or precipitate may be asymmetric or irregular in appearance compared with cocci, which should be symmetric, smooth-walled, and uniformly stained.12
What features are considered ‘abnormal’ on ear cytology?
- Leukocytes: The presence of leukocytes, especially neutrophils, may indicate infection. They gain access to the lumen via exudative inflammation, epithelial ulceration, or extension from the tympanic cavity.12 Noting the presence of leukocytes on serial cytology can help to monitor disease progression or response to therapy.12 The presence or absence of bacteria should be noted, as sterile inflammation could indicate other differential diagnoses, like allergic contact reactions or pemphigus foliaceus.12
- Malassezia: Look for the characteristic peanut, snowman, or shoeprint shape due to unipolar budding.12 Malassezia pachydermatis is the predominant species, although culture and speciation are not considered clinically relevant.12 Mean counts of 5 or more per high-dry field (40x) in dogs or 12 or more per highdry field in cats is considered abnormal; 2 or less per high-dry field is considered normal in both dogs and cats.12
- Bacterial cocci or rods: Pathogenic bacteria typically identified are coagulase-positive Staphylococcus (pseudintermedius, schleiferi ssp coagulans, aureus, some coagulase-negatives can be pathogenic—eg, schleiferi ssp schleiferi), Pseudomonas, and Proteus.12 Finding rods in the absence of inflammation may suggest Corynebacterium, which can be found in a normal ear canal and are not considered pathogenic.12,14,15 Cytology lacks the ability to speciate bacteria, but it can often be clinically assumed that cocci are Staphylococcus.12,16 Mean counts of ≥25 per highdry field in dogs or ≥15 or more per high powered field in cats is considered abnormal.2
- Parasites: Otodectes cynotis, an ear mite, is not species specific and is contagious among animals. It is more commonly a cause of otitis externa in cats than in dogs, whether through mite burden or types 1 and 3 hypersensitivities.12 Demodex ssp, Otobius megnini, Sarcoptes scabiei or Notoedres cati, Eutrombicula alfreddugesi, and Neotrombicula autumnalis may also infect the external ear.12,2
Is a culture helpful in otitis media?
Pending the WAVD consensus guidelines, the authors’ opinion is that culture of the external ear is neither necessary nor helpful for most cases of otitis externa. The systemic minimum inhibitory concentrations (MICs) reported on susceptibility testing are not clinically relevant to topical application, as the concentration achieved with topical therapy ranges from tens to thousands of times greater.17 Many topical medications (eg, mupirocin, neomycin, polymyxin B, silver sulfadiazine) are not tested on standard cultures. Systemic therapy will not reach otitis externa as the infection is contained within a cartilage tube with poor vascular supply.12
For otitis media, culture is strongly indicated. Cultures should be submitted to a laboratory that will speciate all Staphylococcus, regardless of tube coagulase status.18 Suspicion for otitis media can be based off:
- diagnostics: tympanic membrane is discolored, absent, or bulging; fluid visible behind the tympanum; the malleus is not apparent; mass effect; other abnormalities identified on imaging3,5
- history: chronic recurrent otitis that is not responding to appropriate empirical therapy (the authors suggest a 2-strikes rule for first-line antibiotics) or with concurrent neurologic signs19
Cytology and culture of the middle ear are necessary to definitively diagnose otitis media and guide systemic antibiotic therapy.1 Cytology is recommended to confirm the presence of organisms in the submitted sample and that culture results are consistent with what is seen cytologically. It is important to note that the bacterial population within the middle ear can differ from the population in the external canal in up to 89.5% of cases.1 This reinforces that empiric choices of systemic antibiotics for some severe/ neurologic otitis media cases can be started based on external ear cytology. However, ideally, a middle ear culture would be obtained for the best targeted treatment.
How is a middle ear culture obtained?
When a patient is under anesthesia, the tympanic membrane is visualized. If the tympanic membrane is intact, then the external ear canal should be flushed thoroughly before a myringotomy is performed in order to collect as specific of a sample as possible.1,21 A sterile cone is passed to the tympanic membrane with a handheld otoscope, and a sterile swab is passed into the middle ear through the caudoventral portion of the pars tensa in order to avoid the germinal epithelium over the manubrium and to avoid the oval and round windows.1
With a video otoscope, a beveled tomcat catheter or a spinal needle is used through the working channel, and a 12-mL syringe is attached.3 Immediately after puncturing the tympanic membrane using the bevel, 1 mL of saline is flushed into the middle ear and aspirated back.3 After the sampling and rechecking the endotracheal tube cuff, the middle ear is gently flushed with saline (eg, using a 3.5 French red rubber catheter and a 12.0-mL syringe or a VETPUMP system).21 Complications of overaggressive or inaccurate cleaning can include excessive pain, vestibular symptoms, symptoms of facial nerve injury, partial deafness, or iatrogenic otitis interna. Cats can be highly susceptible to developing Horner syndrome following flushing due to submucosal, postganglionic, sympathetic nerve fibers that pass near the cochlear promontory.1 All fluid should be suctioned out, and a nonototoxic drying agent (eg, boric acid, acetic acid, salicylic acid, malic acid, etc.) or topical steroid can be applied.1 Following myringotomy, systemic medications can be started or continued, such as steroids for inflammation and pain or empiric antibiotics based on cytology pending culture results. A recheck cytology and otoscopy should be scheduled 3 and 6 weeks postprocedure to ensure appropriate resolution of infection and healing of the tympanic membrane.5 The tympanic membrane should heal within 21 to 35 days if the area is free of infection and debris.3
What types of imaging can be used for the ear? Imaging can determine involvement of the middle or inner ear, differentiate between peripheral vs central vestibular conditions, differentiate between infectious or inflammatory and neoplastic processes, show changes consistent with chronicity, assess involvement of adjacent structures, and screen for postsurgical complications.20 Imaging is part of the diagnostic work-up of otitis media as it can be clinically indistinguishable from otitis externa in the absence of neurologic abnormalities.22
Common types of imaging used are as follows:
- Radiographs: Although plain film radiographs plus or minus canalography are the most accessible, they require specific positioning under general anesthesia to obtain diagnostic quality images and can be challenging to draw meaningful interpretations.20 The authors do not perform this diagnostic as the costs outweigh the benefits.
- Computed tomography (CT): CT is useful for evaluation of otitis externa and otitis media, as well as nasopharyngeal polyps, tumor and lymph node staging of neoplasia, and evaluation of fistulous tracts or abscesses.20 CT is often the preferred modality, even in humans, because of its greater sensitivity than radiographs, better availability, lower cost, and faster imaging process than magnetic resonance imaging.20,22
- Magnetic resonance imaging (MRI): MRI is generally less indicated for otitis but may be more helpful in the presence of neurological signs, such as differentiating between central and peripheral vestibular disease.20 This is more commonly performed under the consult and care of a neurologist than a dermatologist.
What about prevention rather than treatment?
Otoscopy, cytology, and advanced imaging of the external and middle ear mostly address the short-term perpetuating causes of infectious otitis. However, identifying and addressing the underlying cause is necessary to prevent chronic, recurrent cycles of otitis externa that can lead to end-stage ear disease, discomfort, decreased quality of life, and client frustration.1,12 Treating infectious otitis without addressing and managing primary factors will result in treatment failure.12 The hunt for primary causes should include evaluation for atopy, food allergies, endocrine disease, etc, as determined based on the clinical picture.1 Specific diagnostics may include abdominal ultrasound, complete blood count, chemistry, urinalysis, baseline cortisol, thyroid levels, skin cytology, fungal culture, diet trial, and intradermal and serum testing for environmental allergies.
What happens when the patient isn’t responding to appropriate first-line treatments?
Don’t let the snowball get out of control. Referring to specialists earlier offers a better prognosis for the patient, hence the suggested 2-strikes rule for empiric antibiotics. The ear is an incredibly unforgiving organ. Whereas the skin may have additional treatment options due to its accessibility, options for the ear are more limited, particularly with the brain nearby. The resultant avalanche of chronic irreversible changes, antibiotic resistance, and neurologic signs can be dangerous, difficult, and expensive for the patient.
In a study of 65 dogs with chronic otitis, dogs treated by board-certified veterinary dermatologists in addition to primary care veterinarians had better long-term outcomes (lower median rate of otitis recurrence, complete resolution of otitis signs, resolution of otic proliferative changes) than those that were not referred and treated by primary care veterinarians alone.23
As a general guideline, the authors recommend specialist referral in at least these situations:
- Failed 2 attempts at medical management of the otitis (eg, before reaching for 3rd-line/ compounded antimicrobials)
- Has not resolved with treatment after 2 to 3 months
- Recurrent otitis (>3 episodes per year)
- Suspected/confirmed otitis media
References
- Angus JS, Campbell KL. Uses and indications for video-otoscopy in small animal practice. Vet Clin North Am Small Anim Pract. 2001;31(4):809-828. doi:10.1016/ s0195-5616(01)50072-8
- Rosser EJ Jr. Causes of otitis externa. Vet Clin North Am Small Anim Pract. 2004;34(2):459-468. doi:10.1016/j. cvsm.2003.10.006
- Cole, LK. Otoscopic evaluation of the ear canal. Vet Clin North Am Small Anim Pract. 2004;34(2):397-410. doi:10.1016/j. cvsm.2003.10.004
- Njaa BL, Cole LK, Tabacca N. Practical otic anatomy and physiology of the dog and cat. Vet Clin North Am Small Anim Pract. 2012;42(6):1109-1126. doi:10.1016/j. cvsm.2012.08.011
- Radlinksy MG. Advances in otoscopy. Vet Clin North Am Small Anim Pract. 2016;46(1):171-179. doi:10.1016/j. cvsm.2015.08.006
- Murphy KM. A review of techniques for the investigation of otitis externa and otitis media. Clin Tech Small Anim Pract. 2001;16(4):236-241. doi:10.1053/ svms.2001.27601
- Fan TM, de Lorimier LP. Inflammatory polyps and aural neoplasia. Vet Clin North Am Small Anim Pract. 2004;34(2):489- 509. doi:10.1016/j.cvsm.2003.10.008
- Cole LK. Primary secretory otitis media in Cavalier King Charles spaniels. Vet Clin North Am Small Anim Pract. 2012;42(6):1137-1142. doi:10.1016/j. cvsm.2012.08.002
- Swales N, Foster A, Barnard N. Retrospective study of the presentation, diagnosis and management of 16 cats with otitis media not due to nasopharyngeal polyp. J Feline Med Surg. 2018;20(12):1082-1086. doi:10.1177/1098612X17746282
- Cook LB. Neurologic evaluation of the ear. Vet Clin North Am Small Anim Pract. 2004;34(2):425-435, vi. doi:10.1016/j. cvsm.2003.12.001
- Strain GM. Canine deafness. Vet Clin North Am Small Anim Pract. 2012;42(6):1209-1224. doi:10.1016/j. cvsm.2012.08.010
- Angus JC. Otic cytology in health and disease. Vet Clin North Am Small Anim Pract. 2004;34(2):411-424. doi:10.1016/j. cvsm.2003.10.005
- Griffin JS, Scott DW, Erb HN. Malassezia otitis externa in the dog: the effect of heat-fixing otic exudate for cytological analysis. J Vet Med A Physiol Pathol Clin Med. 2007;54(8):424-427. doi:10.1111/j.1439-0442.2007.00938.x
- Henneveld K, Rosychuk RA, Olea-Popelka FJ, Hyatt DR, Zabel S. Corynebacterium spp. in dogs and cats with otitis externa and/or media: a retrospective study. J Am Anim Hosp Assoc. 2012;48(2):320-326. doi:10.5326/JAAHA-MS-5791
- Korbelik J, Singh A, Rousseau J, Weese JS. Characterization of the otic bacterial microbiota in dogs with otitis externa compared to healthy individuals. Vet Dermatol. 2019;30(3):228-e70. doi:10.1111/ vde.12734
- McKeever PJ, Torres SM. Ear disease and its management. Vet Clin North Am Small Anim Pract. 1997;27(6):1523-1536. doi:10.1016/s0195-5616(97)50137-9
- Boyd M, Santoro D, Gram D. In vitro antimicrobial activity of topical otological antimicrobials and Tris-EDTA against resistant Staphylococcus pseudintermedius and Pseudomonas aeruginosa isolates from dogs. Vet Dermatol. 2019;30(2):139-e40. doi:10.1111/vde.12717
- . Morris DO, Loeffler A, Davis MF, Guardabassi L, Weese JS. Recommendations for approaches to methicillin‐resistant staphylococcal infections of small animals: diagnosis, therapeutic considerations and preventative measures: Clinical Consensus Guidelines of the World Association for Veterinary Dermatology. Vet Dermatol. 2017;28(3):304-e69. doi:10.1111/vde.12444
- Gotthelf LN. Diagnosis and treatment of otitis media in dogs and cats. Vet Clin North Am Small Anim Pract. 2004;34(2):469-487. doi:10.1016/j. cvsm.2003.10.007
- Bischoff MG, Kneller SK. Diagnostic imaging of the canine and feline ear. Vet Clin North Am Small Anim Pract. 2004;34(2):437-458. doi:10.1016/j. cvsm.2003.10.013 21. Cole L, Nuttall T. Clinical Techniques: When and how to do a myringotomy – a practical guide. Vet Dermatol. 2021;32(3):302-e82
- Cole L, Nuttall T. Clinical Techniques: When and how to do a myringotomy – a practical guide. Vet Dermatol. 2021;32(3):302-e82.
- Belmudes A, Pressanti C, Barthez PY, Castilla-Castaño E, Fabries L, Cadiergues MC. Computed tomographic findings in 205 dogs with clinical signs compatible with middle ear disease: a retrospective study.Vet Dermatol. 2018;29(1):45-e20. doi:10.1111/vde.12503
- Logas DB. Treatment outcomes for chronic canine otitis externa in primary care and dermatology specialty practice settings. Abstracts of the North American Veterinary Dermatology Forum, April 13–16th, 2011 Galveston, Texas, USA. Vet Dermatol. 2011;22(3):289-304.

