The ABCs of veterinary dentistry: When waiting is wishful thinking
When it comes to dental care, sometimes immediate action is a must for your patient’s health and comfort.
Sometimes waiting to perform treatment is the best course of action when a patient presents with dental concerns, as noted in the August issue of dvm360® (“The ABCs of veterinary dentistry: W is for waiting to treat”). But other times waiting is simply not an option—the patient’s problem needs to be addressed immediately.
Missing teeth
Dogs should have 42 permanent teeth, cats 30. If 1 or more teeth are not present clinically, it is time for detective work This involves examining intraoral radiographs to determine whether a tooth is present subgingivally and, if so, whether a pathologic process (periapical lucency) is at play that needs immediate care. Waiting to diagnose and treat can lead to progression of subgingival pathology in these patients (Figure 1).
Figure 1a: Clinically missing left mandibular first premolar in a 7-month-old dog.

Figure 1b: Radiograph showing the first premolar present but unerupted.

Figure 1c: Operculectomy was performed to remove thickened gingiva, exposing the premolar and creating a path for eruption.

Figure 1d: Clinically missing left mandibular first premolar in a mature dog.

Figure 1e: Radiograph showing an unerupted first premolar that created a dentigerous cyst requiring oral surgery.

Persistent primary teeth
When a patient presents with persistent primary teeth—primary (baby) and secondary (adult) teeth present clinically in the same alveolus—immediate extraction of the primary tooth is indicated. Persistent primary teeth may overcrowd the dental arch, moving the secondary teeth to abnormal locations and causing oral discomfort. Double sets of roots may also prevent normal development of the alveolus and periodontal support around each permanent tooth, leading to early tooth loss.
A persistent primary tooth should be extracted as soon as the permanent tooth is observed to erupt in the same alveolus. When extraction is performed early, the abnormally positioned permanent tooth ideally moves into normal position. Extraction must be done carefully to avoid accidental damage to the unerupted, permanent canine tooth that lies lingual to the mandibular teeth and rostral to the maxillary deciduous canines. Avoid placing the elevator along the lingual surface of the mandibular deciduous teeth. Instead, only elevate along the mesial surface (front), labial surface (toward the lip), and distal surface (caudally) of the mandibular deciduous teeth, and buccally and distally around the maxillary deciduous canines. Examination of intraoral radiographs before extraction is important to confirm that the tooth about to be extracted is a primary tooth (Figure 2).
Figure 2: Persistent primary right maxillary canine tooth causing swelling and rostral displacement of the secondary canine.

Fractured deciduous canine teeth
Normally, deciduous canines exfoliate by 6 months of age. Occasionally, the crowns fracture secondary to chewing on hard objects. Waiting to extract a fractured deciduous tooth can lead to periapical infections and discomfort (Figure 3).
Figure 3: Bilaterally fractured maxillary deciduous canines. Extractions are indicated as soon as possible.

Discolored teeth
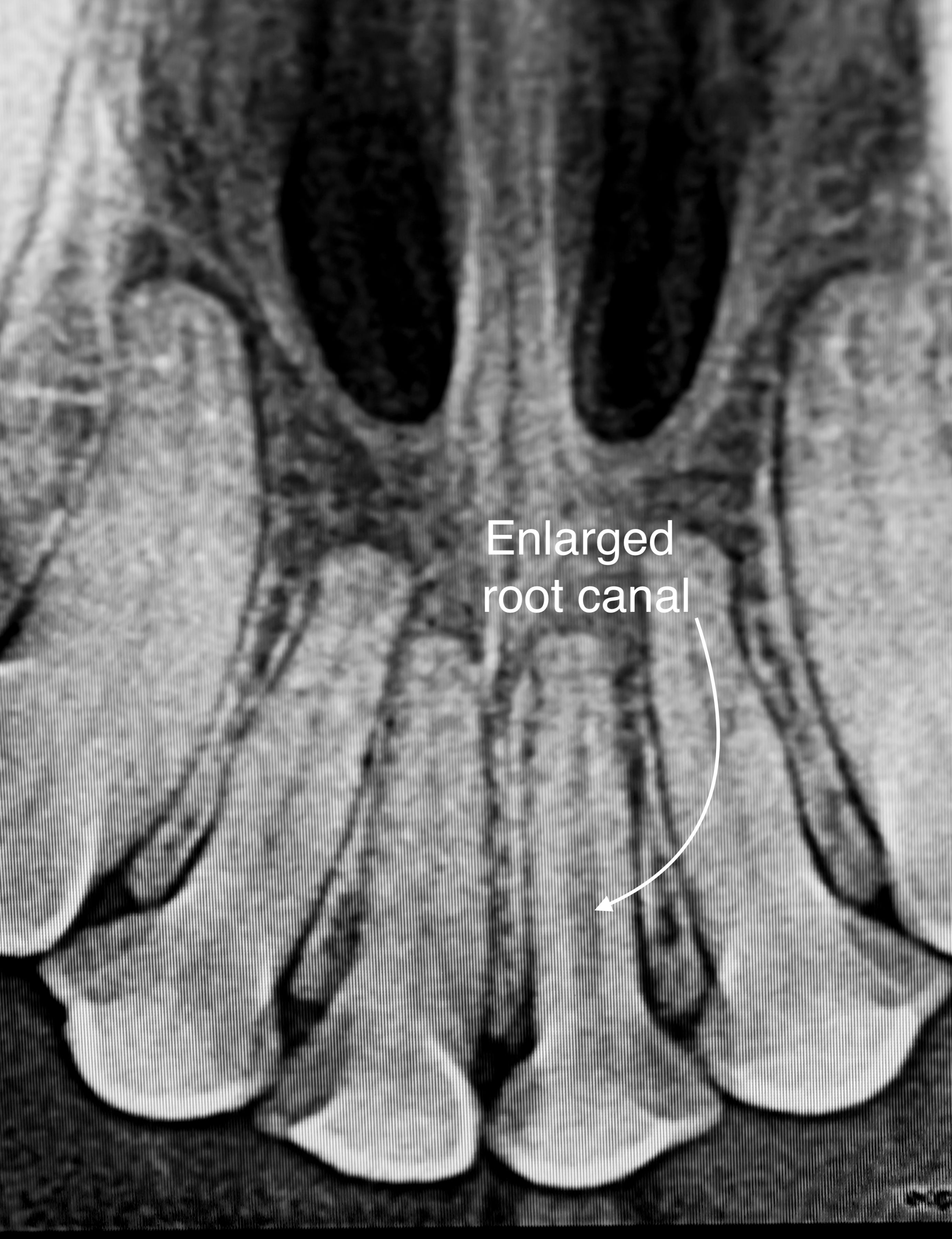
Discolored teeth are considered nonvital. Discoloration commonly occurs secondary to concussive or thermal trauma that results in internal bleeding and pulpal necrosis. Dull pain is reported by humans from pulpitis in discolored teeth. The treatment of choice for discolored teeth in dogs and cats is either root canal therapy to remove the nonvital pulp or extraction (Figure 4).
Figure 4a: Discolored left maxillary first incisor.

Figure 4b: Radiograph showing an enlarged root canal consistent with a nonvital tooth. Extraction or root canal therapy is indicated.
Complicated tooth fractures
Once the pulp is exposed via fracture, oral bacteria infect the area, causing inflammation and pain. If left untreated, the pulp eventually will necrose, leaving an open portal for bacteria to populate the periapical tissues and cause pain. When diagnosed early and treated within 48 hours of the fracture, the tooth may be saved through vital pulp therapy. After 48 hours in the mature dog or cat, either root canal therapy or extraction is the treatment of choice.
Facial swelling after tooth fracture
When an adult maxillary cheek tooth is fractured with pulp exposure, the area below the eye often swells. When this occurs, administering antibiotics and anti-inflammatories usually results in temporary resolution. Within days to weeks, however, the swelling returns because it is secondary to complicated cheek teeth fractures with open pulp chambers. Successful treatment in these cases involves root canal therapy or extraction of the fractured tooth (Figure 5).
Figure 5a: Facial swelling below the left eye caused by a complicated fracture of the left maxillary fourth premolar.

Figure 5b: Root canal therapy or extraction is indicated as soon as possible.

Plaque and tartar with inflammation
Once plaque and tartar result in gingival inflammation, it is time for professional dental scaling, irrigation, and polishing under general anesthesia. Treatment in these cases should not wait until the annual dental exam.
Tooth resorption that is exposed into the oral cavity
We still do not know the cause of external tooth resorption in dogs and cats, but we do know that once the resorption is exposed to the oral cavity, bacteria invades the pulp and causes inflammation and pain. Waiting, antibiotics, and anti-inflammatory medication are not indicated. Extraction is the treatment of choice.
Feline gingivostomatitis
The etiology of gingivostomatitis is believed to be multifactorial. This creates a challenge for any successful treatment other than full-mouth or selective extractions. In rare mild cases, stringent plaque control and a change in diet may be curative. Treating with repositol steroids or anti-microbials is wishful thinking with only short-lived improvement. In cases of refractory stomatitis despite extractions, CO2 laser ablation, with or without every-other-day oral prednisolone administration, shows promise in relieving inflammation (Figure 6).
Figure 6a: Marked inflammation surrounding a cat’s left mandibular cheek teeth.

Figure 6b: Resolution 6 months after full-mouth extraction.

Overcoming client concerns
Expense
Thanks to wellness plans that include dental evaluation, scaling, polishing, and full-mouth intraoral imaging, fees for needed dental care are less of an issue than they once were. Clients who understand the ramifications of dental disease and believe their dog or cat needs dental care will find a way to afford it. In-clinic and third-party payment plans are an option for most clients, and many pet insurance plans cover dental diseases as long as the pet was covered before the diagnosis was made.
Anesthesia
Some clients are hesitant to proceed with recommendations because they fear general anesthesia will harm their pet. Thanks to Fear Free preanesthetic patient evaluation geared to the individual patient’s age and condition, patient-tailored preanesthetic and induction medication regimens, and close anesthesia monitoring during and after the procedure, anesthesia is considered safe with only rare adverse events.
Waiting in most of the cases outlined here is not wise and can lead to harm. When the moment of truth occurs during an oral exam, it is wise to be proactive in advocating for your patient. Your patient and client will thank you.
Dr. Jan Bellows owns All Pets Dental in Weston, Florida. He is a diplomate of the American Veterinary Dental College and the American Board of Veterinary Practitioners. He can be reached at dentalvet@aol.com.
